Patient Education

Patient Education
Patient Education Library
The RevenueWell Patient Education Library provides the most popular topics in dentistry that will help you better maintain your dental health. Select an article or video below to get started now.
Articles
Videos
Your Child's First Dental Visit new
Keeping Your Child Calm For Their Dental Visits

While adults may dread the slow and steady approach of an impending dental visit, that same sort of trepidation doesn’t have to be part of a child’s experience.
Most of the fear we’ve amassed about a trip to the dentist is, unfortunately, learned behavior. Just as it is with food and music preferences, our fears are often conveyed upon us by our friends and family. Dentists are trained at calming their patients, and pediatric dentists even more so. In fact, pediatric dentists have, on average, two to three years of additional training beyond their four-year dental program, so they can address the specific needs of pediatric patients.
Stop the Fear Mongering
We all know kids are experts at mirroring. The moment that inappropriate word exits your mouth, it’s been filed away for future use by your precocious two-year-old … they hear and see everything! So, just as it is with foul language, you’ve got to shelter your fears of the dentist from your kids, and save the stories of angst for the ears of adults only.
Can’t hold back? Then, be prepared to wrestle with your kids every four to six months when their scheduled visit arrives. Kids aren’t afraid of the eye doctor’s glaucoma, dye, and numbing experiments, nor should they be afraid of the procedures performed on their teeth.
Address Questions, but Limit Details
Once your children have reached a certain age, they’re going to grow curious about their dental visit. Help them with this natural curiosity by addressing what’s less intimidating: things like what the office might look and smell like, that they’ll be in a special chair, and that there will be a lot of light to see inside their mouths. The more complicated (and specific questions) should be left to your doctor, as they have very unique and often playful ways to address these questions.
Ask the Dental Office Staff for Advice Prior to Visiting
Sometimes, a little prep work goes a long way. And who better to ask for advice than the friendly men and women who welcome you to the office?! Tiny things like making your appointment early in the morning, talking about your own positive experiences, bringing a toy, or even allowing your child to go in for their cleaning without you being there, can empower your child in ways you might not foresee. So, ask away, the office staff is there to help!
Bringing your children to the dentist can be simple if you take heed to follow these few simple steps. Start early, talk about good oral health, and follow your own advice. In no time, you’ll have a family without a fear in the world when it comes to the dentist.
Dentures Partial Dentures
A smile just isn’t a smile if it’s incomplete.
Missing teeth cause a host of problems, from difficulty speaking and eating to low self-confidence to jawbone deterioration.
Don’t give up on your smile.
Advances in dental materials and technology have made full and partial dentures more lifelike and comfortable than ever.
Depending on how many natural teeth you still have, your doctor may recommend a complete (full) or partial denture.
- Partial dentures are used to fill in the space created by missing teeth to fill out your smile.
- Complete dentures are used to completely replace all teeth.
If you prefer a secure full or partial denture, and do not want clips or adhesive, then consider implant-supported dentures.
In a brief surgery, an implant dentist can secure a few dental implant posts to hold your dentures in place. With implant-supported dentures, you won’t have to worry about slippage, and your prosthetic will feel safe and sound.
Now that I have dentures, do I still need to visit a dentist?
Regular appointments with the dentist are as important for denture-wearers as for people with natural teeth. The mouth tissue, bony ridges and gums that support dentures are constantly undergoing changes and may impair the denture’s proper function.
Even such general health ailments as vitamin deficiencies, extended illness, drug therapy, weight loss, diabetes or high blood pressure can change the way dentures fit.
Ill-fitting dentures can seriously damage the mouth, causing abrasions, bruises, inflammation and rapid destruction of the supporting bone. Prolonged irritation of this kind may result in the development of tumors.
It is important to have a dental checkup at least once a year to insure that your dentures are properly adjusted and that your mouth is in good health.
Tooth Extractions: Post-Op Instructions
Tooth Extraction: Post-Operative Instructions
After a tooth extraction, the healing process begins. A blood clot must form to stop any bleeding and protect the empty socket. Bite down on a piece of gauze for 30-45 minutes immediately after your extraction. If bleeding or oozing persists, switch to a clean gauze pad and bite down for another 30 minutes. Continue this until the blood flow stops and a clot is formed.
One of the most crucial aspects of post-tooth extraction care is to not dislodge the clot. Avoid using drinking straws, rinsing vigorously, smoking, brushing near the extraction site, or drinking alcohol for at least three days. These actions may dissolve or disrupt the clot, leading to delayed healing. Also, refrain from engaging in vigorous exercise for the first two days, as this could increase blood pressure and potentially lead to increased bleeding.
You may experience some mild pain and swelling after tooth extraction. Ice packs can minimize swelling for the first 40 hours. Pain medications should be taken as directed. Contact your dentist or oral surgeon for guidance if they do not work. If antibiotics are prescribed, take the entire dose even if there are no signs of infection.
Drink lots of fluids, eat nutritious, soft foods for the first two days, and avoid crunchy or hard foods until you feel up to it.
After the first 24 hours, it is crucial to return to your normal oral hygiene routine. This should include brushing twice daily and flossing once daily. After a few days, you should feel ready to return to your normal activities. If your pain increases or you experience heavy bleeding or increased swelling after the first three days, call your dentist or oral surgeon immediately.
Wisdom Teeth
Wisdom Teeth
Wisdom Teeth are the third and final set of molars that most people get in their late teens and early twenties. When these teeth are aligned correctly and healthy, they can be a part of a healthy mouth. However, most wisdom teeth are misaligned and need to be removed.
Your dentist may recommend removal of your wisdom teeth if there are signs of pain, infections, damage to adjacent teeth, gum disease, tooth decay or cysts. Your dentist may also recommend removing your wisdom teeth without any of these systems in order to avoid a more difficult procedure later on.
Wisdom Teeth Removal Procedure
A typical surgery to remove wisdom teeth requires sedation and may lead to facial swelling and bleeding for a few days afterwards. There are two potential complications that can happen after surgery: dry socket and paresthesia.
- A dry socket is a complication from surgery that occurs when a blood clot either fails to form or is dislodged. This will delay healing time, but can be treated by your dentist placing medication in the socket.
- Paresthesia occurs less frequently than a dry socket, but is a numbness of the tongue, lip, or chin that happens if nerves are bruised or damaged during the tooth removal service.
Regular Dental Checkups
Regular dental checkups allow your dentist to keep an eye on your wisdom and make recommendations about what would be the best course of action to keep your mouth healthy.
7 New Tips to Prevent Gum Disease
To avoid gum disease, a solid oral care regime is imperative
Brush twice a day, floss at night, and use mouthwash. This is the familiar refrain, so let’s step away from that simple 3-step plan and look at other ways to prevent gum disease. Gingivitis and its advanced cousin, Periodontal disease, are silent offenders. Most often, you may not even know you should be concerned. After all, the serious problems take place beneath your gum line where you can’t see them.
Plaque and gum disease can also influence and exacerbate conditions
A growing number of scientists believe that conditions like heart disease and stroke can be influenced and exacerbated by plaque and gum disease – conditions we do not want to encourage by a lack of attention to good oral hygiene.
Seven easy things you can do to help protect your mouth from gum disease
1. Eat More Chicken! This is more than just a prominent fast food slogan. Consuming more chicken, as well as other meats, cheeses, nuts, and milk does a body good. All are believed to provide your teeth with calcium and phosphorous needed to remineralize enamel after it’s been bombarded by the acids that cause tooth decay.
2. Eat more Veggies! Everyone knows we need more vegetables in our diets. Our waistlines and our teeth love them for their water content, as well as their vitamin and mineral profiles. There’s no doubt about it, veggies are good for you. Not a big fan? Incorporate them into soups, or in a great fruit smoothie … you won’t notice the difference, but your teeth and gums will.
3. Use an anti-microbial mouthwash: The key here is using a mouthwash that is anti-microbial. Find one you’ll actually use every day, and use it once in the morning after brushing, and again after brushing before bed. Try to find one that’s low in alcohol or without it altogether, as alcohol dries out your mouth and can contribute to tooth decay. More saliva equals better oral health.
4. Try a toothbrush that moves: Get adventurous and test out an electronic toothbrush that’s been endorsed by the American Dental Association (ADA). These toothbrushes are more effective than you’ll ever be at removing plaque and bacteria, and will protect your gums from aggressive brushing.
5. Chew Gum! Keep that saliva flow going after a meal with sugar-free gum that contains Xylitol — a natural sweetener derived from plants. It doesn’t break down like sugar, and can help keep a neutral pH level in the mouth. If you want to avoid Aspartame in your Xylitol chewing gum, search online or ask your dentist. It’s difficult to find gum without Aspartame these days, but such a product does exist.
6. Get Braces! That’s right, getting braces can help protect you from gum disease. Crooked teeth are great enablers of tooth decay, which can lead to gum disease by allowing bacteria and plaque to colonize in the areas where your teeth are not aligned. Getting your teeth aligned eliminates these hideouts where your toothbrush cannot reach, all while straightening your smile at the same time.
7. Quit Smoking! This one is always worth mentioning. Smoking is always bad for your body, your gums, and your teeth.
Dont Like Flossing Try One Of These Methods and Get Those Gums in Shape
Don’t Like Flossing? Try One Of These Methods and Get Those Gums in Order!

When it comes to dental floss, what’s the best kind? If you ask a dentist, they’ll tell you the best dental floss is the floss you’ll actually use! That could be Teflon floss, dental tape, nylon floss, waxed floss, and flosses with or without flavors – there are a lot of choices! There are also a number of ways to get your flossing done that don’t have you wrapping a long string of floss across your fingers and deftly maneuvering your hands in such an enclosed space.
Dental Pick
If you’re prone to ignore flossing, you may want to consider a good ol’ fashioned dental pick. They look kinda’ like a plastic toothpick with a strand of dental floss strapped across a wide u-shaped tip. The simplicity and compact nature of these little portable floss picks seem to add to their convenience, and kids seem to love them when they’re first learning to floss.
Electric Flossers
Depending on the brand, electric flossers are known by a variety of names, and searching for these handy little devices can be somewhat maddening online. From vibrating flossers to power flossers to air flossers, picking the one that’s right for you depends on the task at hand. Power flossers and air flossers seem best if you’re dealing with space concerns near the gumline, and may be a good substitute for an interproximal toothbrush. A vibrating flosser, on the other hand, looks much like a dental pick and because of its design, can cover the entire length of the tooth. Ask your dentist which is best for you.
Oral Irrigator
An oral irrigator is a device that uses a pulsating stream of water to remove plaque and food debris from between your teeth. There are a variety of instruments on the market, and your dentist can recommend one based on the health of your gum tissue and budget. Oral irrigators are remarkably effective at keeping gum tissue healthy, and have been shown to reduce pocket depth due to periodontitis. Pocket depth refers to the depth of the gum tissue that immediately surrounds your teeth. You may not know it, but that’s what your dentist or hygienist is testing for when they’re poking that instrument in your mouth during an exam and calling out numbers!
It’s worth noting that each of these devices, while recommended, should be considered as supplements to normal flossing – still your best choice. But, if you have dexterity concerns, are purchasing something for a youngster, or just want to ensure your teeth are the cleanest they can be, these tool are great options!
Cracked Teeth Causes Symptoms and Treatment

With people living longer and more stressful lives, cracked teeth are seen more and more often at the dentist’s office.
Yet cracked teeth can be difficult to detect for a number of reasons, most notably that the pain often comes and goes. Because of the short periods of erratic pain, it can be difficult to discern which tooth is the culprit.
Is a Cracked Tooth Literally “Cracked?”
A cracked tooth is simply a tooth that has a crack or fracture running along the length of the tooth.
Older teeth, or teeth that are otherwise compromised, are usually susceptible to cracking. In particular, teeth that have fillings have a tendency to crack because they are already weakened from the filling itself.
How Does It Happen?
One of the main causes of cracked teeth is eating hard foods, especially hard candies. Biting down on hard foods puts undue stress on your teeth, eventually causing a crack to form.
Clenching or grinding teeth at night can also cause cracks.
Why It Needs To Be Fixed
When the exterior of a tooth cracks, it causes the inside of the tooth, or pulp, to become irritated. Because pulp is comprised of tissue that includes blood vessels and nerves, this irritation generally leads to pain and discomfort.
Biting pressure that is quickly released can also cause a pinching of the pulp, which results in a quick, sharp pain. Over time more irritation to the pulp can lead to infection of the tissue with even larger problems in store.
It is important to know the signs of a cracked tooth so that you can prevent significant damage from occurring. If you feel a sharp pain when biting down on a hard food, or have sensitivity when your tooth is exposed to heat or cold, then chances are you may have a cracked tooth.
Although cracks might only cause minor discomfort to begin with, it is still a good idea to have your dentist check things out. Depending on the size and location of the crack your dentist will decide the best course of action.
Cracked teeth are often fixed with a filling or crown, both of which ensure the tooth is solid. In the case of a more serious crack, your dentist might recommend a root canal or having the tooth extracted – but this is uncommon for a simple cracked tooth.
Acting early can help you to avoid larger problems down the road.
Gum Disease
The most common disease in the United States
The most common disease in the United States is not what you may think. Heart disease, stroke or cancer come to mind, when gum disease is actually the single most prevalent disease in America.
In fact, it affects more people than heart disease, stroke, Alzheimer’s, and cancer combined. About 80% of the population has some form of gum disease, also known as periodontal disease, periodontitis (advanced) and gingivitis (mild).
What is Gum Disease?
Gum disease is an infection of the gums and bone that support teeth. It usually starts early in life and progresses as a person ages.
It all starts when plaque hardens into tartar (also called calculus) below the gum line. This irritates vulnerable soft tissues and infection can set in. Combined with decaying food particles lodged between teeth and bacteria emitted by plaque, the infection can spread quickly.
Symptoms are so mild in the early phase that many patients don’t recognize them: red, tender, swollen gums, bleeding when brushing teeth, slight discomfort while chewing hard foods. As the condition progresses, gums recede from teeth and pockets of bacteria form. The bacteria can destroy gum tissue and bone, causing tooth and bone loss.
Why is Gum Disease So Serious?
Recent research reveals that gum disease is linked to increased risk for major overall health problems, including, but not limited to stroke, heart disease, respiratory problems, osteoporosis, diabetes complications, low birth weight and most recently, dementia.
It makes perfect sense that gum disease is linked to overall health problems. Everything that enters or is present in the mouth has access to the whole body. The mouth is a portal to the body. That’s why regular checkups and hygiene visits are vital to not only oral health, but overall health as well.
Is Gum Disease Curable?
Unfortunately, gum disease is not curable. However, your dentist can detect early warning signs of gum disease at your regular dental checkups.
At this stage, prevention might be as simple as changing your brushing technique, improving your flossing routine or changing the products you use for oral care at home.
Once gum disease sets in, your dentist can often treat it with non-surgical therapy including:
- Scaling or Root Planing – These deep-cleaning measures involve scraping and removing plaque and tartar from teeth above and below the gum line.
- Laser Treatment – Remove bacteria and promote gum reattachment.
- Antibiotics – These and other medications are often used together with scaling and root planing to stop the spread of infection and inflammation in the mouth. They come in several different forms that range from medicated mouthwashes to antibiotic-containing gels or fibers that are placed in gum pockets to slowly kill bacteria and help gums to heal.
- Surgery – advanced cases may require the care of a periodontist.
Expect to attend more frequent hygiene visits so that a dentist or hygienist can monitor your condition and make sure that recovery is on track.
What is Laser Treatment for Gum Disease?
Combined with comprehensive periodontal therapy, a diode laser for soft tissue procedures can remove and reduce some periodontal infection. This type of treatment also promotes reattachment of gum tissue to teeth.
Laser dentistry is precise and conservative in comparison to traditional therapies. Some patients do not even need anesthesia during laser therapy.
Tips for Proper Brushing Habits
Brushing: A Lifetime Habit

Does your child’s brushing more resemble a lumberjack sawing trees in half or a gentle massage? If it’s the former, they may be in for a lifetime of sensitive teeth, bonding treatments, and receding gums.
But not to worry! Now is the perfect time to help them learn to make brushing the right way a habit.
How to Brush?
Teach your littles to brush gently, in short back-and-forth strokes, as well as circular motions, aiming the head of the toothbrush at a 45-degree angle toward the base of the gums. Hit all surfaces of each tooth, not just the ones you can see when you smile in the mirror.
Also, use toothpaste that contains fluoride and is approved by the American Dental Association (ADA). For littles ones younger than three, use just enough to look like a grain of rice; for those older than three, use a pea-sized amount.
And until your child is at least six years old, make sure part of their routine is you taking over the toothbrush to finish the job.
When to Brush?
Twice a day! Morning and evening. In the morning, go with whatever time works for your family. That can be upon waking or after breakfast, or before lunch…just do it! At night, brush right before going to bed so you brush away the day’s ickies.
For How Long?
Most dentists (as well as the ADA) agree that brushing should take about two minutes to make sure you’re brushing adequately enough. A 15-second quick burst is not going to cut it, sadly.
Any Other Tips?
- Make it a family affair. Brush together, make funny faces in the mirror, or have a dance party while brushing
- Associate a song with brushing to help them brush long enough. Just like singing “Happy Birthday” twice is sufficient for hand-washing, figure out what song your child likes (that lasts two minutes) and have them hum it while brushing
- Make it fun with a special app!
- Choose the right toothbrush
- Practice on a toy
- Drop unnecessary dental habits
We know tooth brushing can be a very difficult chore for some kiddos. Most adults have a hard time brushing adequately as well! But do your best to instill healthy habits now for a lifetime of good dental health. You got this!
Fluoride and Floss What You Need to Know
February is National Children’s Dental Health Month!
This year’s slogan hits two very important concepts for keeping our kids’ dental health in tip-top shape. The 2018 slogan is: “Brush your teeth with fluoride toothpaste and clean between your teeth for a healthy smile.” Yes, it’s a no-brainer to say, but actually doing it takes a little bit of effort. We know, ahem, adults who still don’t floss … so let’s get that positive habit started early!
What you need to know…
Using Fluoride Toothpaste
In the amounts our bodies receive via drinking fluoridated water and brushing our teeth, fluoride is quite harmless and incredibly beneficial for our teeth. It can even reverse the very beginning of tooth decay! Fluoride works by strengthening tooth enamel and making teeth more resistant to acid attacks from plaque, bacteria, and sugars in the mouth.
The American Dental Association recommends using fluoride toothpaste for everyone, including the youngest in our families. As soon as teeth erupt, use a tiny bit (grain of rice size or smaller) of toothpaste on your child’s tooth brush. Then, as soon as they learn how to spit, use a pea-sized amount.
Flossing
How early should your kids start flossing? As early as possible! You know your child best, so when you feel it’s age-appropriate to introduce them to flossing, go for it! The best thing you can do is have your littles watch you floss daily. They see you doing it, they see that it’s not so scary, and they just might want to start copying you.
You may want to have them start with disposable flossers, then move on to regular floss as they get older. And make sure you teach them proper flossing technique! That’s it! Focus on these two things this February, and slowly they’ll become habits that are hard to break.
Hate To Floss? 3 Other Ways to Clean Between Your Teeth
Don’t Like Flossing? Try One Of These Methods and Get Those Gums in Order!

When it comes to dental floss, what’s the best kind? If you ask a dentist, they’ll tell you the best dental floss is the floss you’ll actually use! That could be Teflon floss, dental tape, nylon floss, waxed floss, and flosses with or without flavors – there are a lot of choices! There are also a number of ways to get your flossing done that don’t have you wrapping a long string of floss across your fingers and deftly maneuvering your hands in such an enclosed space.
Dental Pick
If you’re prone to ignore flossing, you may want to consider a good ol’ fashioned dental pick. They look kinda’ like a plastic toothpick with a strand of dental floss strapped across a wide u-shaped tip. The simplicity and compact nature of these little portable floss picks seem to add to their convenience, and kids seem to love them when they’re first learning to floss.
Electric Flossers
Depending on the brand, electric flossers are known by a variety of names, and searching for these handy little devices can be somewhat maddening online. From vibrating flossers to power flossers to air flossers, picking the one that’s right for you depends on the task at hand. Power flossers and air flossers seem best if you’re dealing with space concerns near the gumline, and may be a good substitute for an interproximal toothbrush. A vibrating flosser, on the other hand, looks much like a dental pick and because of its design, can cover the entire length of the tooth. Ask your dentist which is best for you.
Oral Irrigator
An oral irrigator is a device that uses a pulsating stream of water to remove plaque and food debris from between your teeth. There are a variety of instruments on the market, and your dentist can recommend one based on the health of your gum tissue and budget. Oral irrigators are remarkably effective at keeping gum tissue healthy, and have been shown to reduce pocket depth due to periodontitis. Pocket depth refers to the depth of the gum tissue that immediately surrounds your teeth. You may not know it, but that’s what your dentist or hygienist is testing for when they’re poking that instrument in your mouth during an exam and calling out numbers!
It’s worth noting that each of these devices, while recommended, should be considered as supplements to normal flossing – still your best choice. But, if you have dexterity concerns, are purchasing something for a youngster, or just want to ensure your teeth are the cleanest they can be, these tool are great options!
Handling Your Child's Dental Emergency
Oh, No! A Dental Emergency While Away from Home.. Now What?

There are many things that can go wrong when your family is on vacation. You can have a hungry bear rummage through your campsite at night. A thief could steal your purse as they zoom by on a Vespa. Or, you could have a dental emergency, which for some, could make the bear and the thief scenarios seem like child’s play. If your child were to lose a tooth, develop an abscess, or pop a wire in their orthodontics while on vacation, what would you do?
The Scouts Have It Right
The best advice here is, of course, prevention. So, about a month prior to departure – or at least two weeks before you go – schedule a visit to your dentist. There is a lot going on in your child’s mouth that can be seen in a physical exam and through X-rays, so this really is your best course of action. If, however, despite the best of planning you still encounter an emergency while on the road, here are a few steps you can take until you can see your dentist:
Chipped or broken tooth:
First, save any remnants that can be found, and have your child rinse their mouth and the pieces with warm water. If there is bleeding, gauze or a tea bag can be used to enforce clotting. A cold compress can also be used on the cheeks to keep down swelling.
Knocked-out tooth:
Believe it or not, you can actually place a knocked-out tooth right back into the jaw if you’re in a pinch. To do so, rinse off the tooth with warm water (do not scrub it!), holding it by the crown and not the root. Then, be sure the tooth is facing in the correct direction, and place it back in its proper place. If the tooth can’t be reinserted, place it in a small container of milk or water with a pinch of salt, and get to a dentist as soon as possible. In order to save a knocked-out tooth, it should be replaced back in its socket in under an hour.
Lost filling:
Take a stick of sugarless gum (gum with sugar will cause pain) and insert a piece where the filling once was, or you can use an over the counter dental cement until you can get to the dentist.
Broken braces and wires:
Sometimes wires can break and end up poking your child’s mouth. With a good supply of dental wax and the eraser of a pencil, you can fix this problem on your own. Use the end of the eraser to guide the wire back into place, or to a spot where it’s not causing any pain, and then cover the end with wax. Never, ever cut the wire, as it can accidentally be swallowed, or inhaled into the lungs.
Abscess:
An abscess is an infection that occurs in the area surrounding the root of a tooth, or near the gumline. To relieve pain and assist in drawing to the surface the pus that develops, your child can rise with a mild salt water solution of (1/2 teaspoon of table salt to 8 ounces of water) several times a day. Remember though, an abscess is serious, and medical attention is necessary to prevent complications.
Things to Bring with You</4>
- Clove Oil: This pain reducer is your best friend with you have a tooth ache of any sort. It can be purchased at your local health food store for only a few dollars.
- Dental Wax: Can be used for broken or bent orthodontic wires as well as crowns that may have become dislodged. Remember to save the crown so it can later be re-attached.
- Phone Numbers: Bring along the contact info for your child’s dentist and orthodontist, should your family have one, and the number of a recommended dentist in the state to which you’re traveling.
Traveling overseas? These contacts might prove handy
- A local hotel concierge
- The American Embassy in the country you are traveling
- American Military Personnel
- The International Association for Medical Assistance To Travelers — a network of doctors and medical institutions around the world – (www.iamat.org) (716) 754-4883.
- In Europe – American Dental Society of Europe (ADSE) (www.adse.co.uk) Phone: 011 44 141 331 0088
Protecting Yourself Against Oral Cancer

If there were a quick and painless way to identify pre-cancerous cells in the mouth of someone you loved, would you want them to try it? What if that person were you? The truth is, as uncomfortable as it may be to even think of the word “cancer,” thinking about it, and thus detecting it early, is key. That’s why, if you haven’t been to the dentist in a while, you should schedule a visit, because while the oral exam that accompanies your cleaning may not be noticeable to you, it’s often your earliest line of defense in the detection of oral cancer.
Let’s take a quick look at a few of the risk factors and symptoms, and consider a few options you may have to help reduce risk. Keep in mind that no list is exhaustive, and to always share with each of your health care providers your concerns and strategies regarding your oral health.
Those at Risk for Oral Cancer
Passing certain age thresholds and engaging in certain lifestyle habits can place you at increased risk for oral cancer. For example, men tend to have higher rates of oral cancers than women.
Here is the short list:
- Patients age 40 and older (95% of all oral cancer cases)
- Patients age 18-39 who use tobacco, are heavy drinkers, or may have a previously diagnosed oral HPV infection.
Warning Signs
If you experience any of the below symptoms lasting more than 7-10 days, please seek the advice of your doctor. Also, keep in mind that aside from an obviously sore throat, the below symptoms can present themselves in the absence of pain. Look out for changes that can be detected on the lips, inside the cheeks, palate, and gum tissue surrounding your teeth and tongue.
- Reddish or whitish patches in the mouth
- A sore that fails to heal and bleeds easily
- A lump or thickening on the skin lining the inside of the mouth
- Chronic sore throat or hoarseness
- Difficulty chewing or swallowing
Reducing risk
If you do not visit the dentist regularly, you could be missing out on the benefits of early cancer detection. Currently, just over half of all those diagnosed with oral cancer survive more than five years – a statistic driven by late diagnosis – so please visit your dentist and get an oral exam at least once a year. If you are considered “high risk,” (see list above) you should be receiving an oral exam at least every six months, if not more frequently.
Below is a short list of healthy habits you can start doing now, which may reduce your risk.
- Avoid all tobacco products
- Avoid or reduce your consumption of alcohol
- Consume more fruits and vegetables (good for everything, of course)
- Avoid excessive sun exposure that can result in cancer of the lip (using lip balm with an SPF of at least 30 can be helpful)
- Avoid exposure to environmental hazards (wood dust, formaldehyde, printing chemicals)
- Conduct a self-exam monthly so you can catch any of the symptoms listed above. Use a small hand-held mirror so you can see the back of your mouth and tongue
- Consider coffee. While the jury is still out, some research suggests coffee may help protect the mouth from oral cancer.
Oral cancer is serious business. Yet, it can be managed when caught early. So, do the right thing and visit your dentist regularly, and get that screening.
Oral Health and the HPV Vaccine
Teeth Grinding Clenching Bruxism
Understanding Teeth Grinding
While occasional teeth grinding does not usually cause harm, when it happens frequently, teeth can be damaged and other complications can arise.
Role Of Stress in Teeth Grinding
STRESS is a huge factor when it comes to bruxing. In fact, the mouth can show stress before any other area of the body. The more stress, the more bruxing and the harder the bruxing.
Possible Signs and Complications of Bruxism
- Wearing of Teeth – which occurs from movement of the teeth harshly against one another.
- Breaking of Teeth – especially at the edges of front teeth and the cusps or corners of back teeth.
- Sensitive Teeth – usually a generalized soreness and/or cold sensitivity.
- Receeding gums and/or teeth with gum line “notches”
Not everyone has all these problems, and some of these signs take time (usually decades) to materialize.
What should you do about bruxism?
There is not a single cause for bruxism and consequently not a single solution. For a large number of people, the problem is a misaligned bite. Through a series of physiological signals, this triggers a dramatic increase in the amount of bruxing.
If you feel you may be grinding or clenching, please schedule an appointment with your dentist. They would be able to diagnose the reasons and propose some solutions. Options could range from working to reduce stress to helping you procure a mouth guard or an occlusal guard.
How to Prevent Child Tooth Decay
Preventing Tooth Decay in Children
There’s more to preventing tooth decay than just hiding the candy bowl. And it’s important to remember that even though baby teeth will fall out someday, protecting them is very important!
Best Practices for Dental Health
Below is a list of the best things you can do to ensure that your child’s dentist proclaims “no cavities!” at their next visit.
Get enough fluoride!
It’s a fact: fluoride helps prevent tooth decay. The best way for your child to get enough fluoride is through drinking fluoridated water. If you use well water or bottled, ask your dentist about using a fluoride supplement. And using a fluoride toothpaste for all ages is always a must. Your dentist may also offer a topical fluoride treatment at each routine visit.
Snack less frequently
Constant snacking provides the perfect environment for cavity-inducing bacteria to do their work. Got a grazer at home? Try to discern if their snack habit is a result of truly being hungry. If so, try to bulk up meals with healthy fats to make their tummies happier for longer. If snacking because of boredom, or simply because those yummy fruit snacks are visible, try to help your little one find something else to do until the next mealtime.
Limit sugar
Excess sugar in the diet is known to cause a variety of issues for the body and is especially bad for our teeth. Childhood is the perfect time to persuade those taste buds to be happy with whole foods and less sugar. Try cheese sticks, apple slices, or a handful of nuts. All are great choices when it comes to filling tummies without wrecking teeth.
Hydrate with water or milk instead of sugar-sweetened beverages
Sports drinks, sodas, and even 100% juice just aren’t good for little chompers. They simply don’t provide enough nutritional benefit to be worth it.
Start healthy habits early
As soon as those cute little baby teeth pop through the gums, you’ll want to start brushing them. And as soon as they’ll let you, you’ll want to teach your littles how to floss. Make their twice daily dental hygiene routine a priority.
Consider dental sealants
Sealants are hardened plastic shields placed on the chewing surface of your child’s molars and pre-molars. They seal the surface of the tooth and help keep food and bacteria from causing cavities. Dental sealants don’t cost much, match the exact color of your child’s tooth, and are quick and easy to apply. Ask your dentist what other tips they have for your child’s specific situation. We know encouraging healthy dental hygiene habits isn’t easy for our littles, but any little bit helps! You can do it!
Sleep Apnea Treatment Snore Guards
Do you experience headaches upon waking and have trouble shaking that sleepy feeling during the day?
Maybe you doze off during meetings or while watching TV? You may suffer from obstructive sleep apnea, a potentially dangerous condition that diminishes restful slumber and may increase your risk of heart attack, stroke and other serious health complications. Your dentist may help you treat sleep apnea with non-surgical oral appliance therapy that alleviates this condition and lets you get the restorative sleep they need.
What is sleep apnea?
Sleep apnea occurs when airflow repeatedly stops for periods of ten seconds or longer. The brain senses lack of oxygen and tells the body to breathe. People with sleep apnea may experience hundreds of these episodes each night and are most likely unaware that it’s happening.
What causes sleep apnea?
When you sleep, the muscles that control your tongue and throat relax. Tissues can sag and restrict airflow, which causes the apnea episode. Sleep apnea sufferers often snore as well, because tissues vibrate as air is forced through narrowed passageways.
Sleep Apnea Treatment
Sleep apnea and snoring could be treated with an easy-to-wear mouth guard (snore guard) that keeps the chin slightly forward to promote optimal airflow. There are a variety of mouth guards available on the market today, and your dentist can help you choose one that is most appropriate for you.
Dental Implants Getting to the Root of Things

With regular dental care and some luck, you may never be a candidate for a dental implant
Knowing about them ahead of time will help inform your decision should the need ever arise. So, what are implants, how do they work, and who needs them?
How Does a Dental Implant Work?
Dental implants are artificial tooth “roots” placed into the jaw to help hold a replacement tooth, bridge, or even dentures, in place.
Typically made of Titanium, which the jawbone will accept or fuse to, dental implants are most often used for patients who have somehow lost a tooth or teeth – whether through accident, injury, or even periodontal disease.
Implants can also help stop periodontal disease from forming by eliminating gaps in the mouth where disease and infection are likely to occur. They prevent the shifting of teeth, which can cause more long-term damage.
Types of Dental Implants
There are two types of implants: Endosteal and Subperiosteal.
Endosteal (in the bone) implants are typically screws, blades, or cylinders that are surgically placed directly into the jawbone. Generally used to support bridges or removable dentures, this type of implant is the most common.
Subperiosteal (on the bone) implants are placed on top of the jaw with posts that protrude through the gum to hold a dental prosthesis in place. These types of implants are used for patients who are unable to wear conventional dentures.
Sometimes an implant is used to anchor orthodontia in place as well.
Dental Implant Candidates
An ideal implant candidate is usually in good health overall, including orally. If you should need an implant, your dentist will likely refer you to an Endodontist, Oral Surgeon, or Periodontist, a professional who specializes in gum tissue and bone in the mouth, to make sure that you have the best care team in place.
Healing time varies, as do success rates – and general post-surgical care is a key component to success.
The Perfect Road Map For Your Child's Oral Health

On July 3rd, 1806, two years into their journey to chart the unchartered west of America, pioneer explorers Meriwether Lewis and William Clark reached a challenge of epic proportion – the Rocky Mountains. What next, they wondered? Without a map, they were forced to do what explorers do – explore, and hope for the best. So, that got us thinking. Wouldn’t it be nice to have a handy map you could use to chart your own dental health? With that in mind, and in honor of our “Dog Days of Summer” explorers, here are a few mile markers you can use to stay on top of your child’s health today, next year, and for years to come!
6 to 24 months
When you’re a new parent, life is a whirlwind, and the dental care of your newborn may not be top of mind when you look in their mouths and see no teeth! But! There are some things you need to know:
Schedule a visit:As soon as that first tooth comes in, you’ll want to schedule a visit and set up a periodic exam schedule. Also, be aware that the ADA recommends fluoridated toothpaste now for all children under the age of 3.
Ask your dentist about:
- Home hygiene basics: Tips and tricks on brushing and other care
- Preventative dentistry: The possible need for fluoride supplements
- Dietary strategies: Achieving a balanced diet early in life for good oral health later
- Feeding practice awareness: Bottle, breast-feeding, and no-spill training cups
- Non-nutritive oral habits: Thumb sucking, pacifiers
2 to 12 years old
Ah, the little ones are growing up. Teeth are coming in at all sorts of crazy angles, and you’re going crazy from the rise in obligations. Here’s a quick list of what to consider during this timeframe:
- Preventative dentistry: Pit and fissure sealants can do wonders for keeping your child’s dental bills down, and their teeth in their head until they’re ready to fall out naturally. Ask about them. They’re affordable AND useful.
- Orthodontic Consultation: Visiting an orthodontist for an early consultation is best done around your child’s seventh birthday. With today’s technology, early intervention can reduce the cost and duration of braces when your child gets older.
The Teen Years
The years “everything” happens! As children start to come into their own, new habits and desires begin to unfold as well. You’ll have to address every imaginable concern during these years, from piercings, to calls for whitening, braces, and the need to refer yourself away from your pediatric dentist and to a general dentist for continuing oral care. So, speak with your dentist about:
- Cosmetic Dentistry: What solutions are advisable now, and what things should be avoided.
- Teen social pressures: Smoking, alcohol, intraoral/perioral piercings and the like
- Orthodontics: Options for minimizing appearance and health problems later in life
- Home hygiene tips: Brushing, flossing, choosing the right mouthwash
- Craniofacial injury prevention: With your children’s possible participation in sports, you’ll want to get them a mouthguard. Hands down it’ll be one of your best investments in a healthy mouth. And skull!
Staying on top of your child’s oral health isn’t as hard as you think, and if you keep this schedule handy, you’ll be ahead of most of your neighbor’s kids when it comes to a healthy mouth and body. Come to think of it … why not share it with them as well? They’ll thank you for the help!
Kicking the Tobacco Habit is Good for your Mouth
Kicking the Tobacco Habit is Good for your Mouth
In the past 50 years the number of Americans who smoke cigarettes has dropped a dramatic 23 percent. However, the risks of tobacco use have not changed. Tobacco is not only dangerous to your heart and lungs, it can also affect your oral health.
More than Just Stained Teeth
From the mild side effects tobacco can cause, including bad breath, tooth discoloration, buildup of plaque and tartar, to the more sinister effects –- including increased risk of oral cancer, loss of bone within the jaw, gum disease and any number of resulting complications — tobacco is an oral health risk.
Tobacco can cause serious health issues by breaking down the attachment of bone and soft tissue to your teeth. Because of this breakdown, the use of tobacco makes smokers much more susceptible to infection and numerous diseases.
In fact, 90% of people who have cancer of the mouth, throat, or gums admit to using tobacco in some form.
Cigarettes, cigars and pipes aren’t the only culprits; smokeless tobacco can be just as detrimental to oral health, if not worse. In fact, there are twenty-eight chemicals found in chewing tobacco alone that are proven to increase the risk of cancer in the mouth, throat, and esophagus.
Chewing tobacco and snuff actually contain higher levels of nicotine than those found in cigarettes and other tobacco products, making it worse for your oral health. Smokeless tobacco can irritate gums causing gum tissue to recede, which exposes the roots, and ultimately makes teeth more susceptible to decay.
Help Is Just Next Door
You don’t have to quit cold turkey. Simply reducing tobacco use is proven to help lower your risks.
Nicotine is a highly addictive chemical and it is often difficult to quit. If you feel that it is time to reduce your risk of cancer, gum disease, infection and other oral complications, your dentist or doctor can help you create a plan to help you quit using tobacco, along with prescribing certain medicines or programs to help you kick the habit.
While the best way to stop is to never start, it’s never too late to quit. Talk to your health professional for best advice on ways to quit using tobacco.
Understanding the Five Stages of Tooth Decay
Understanding Tooth Decay: Five Stages Explained
Did you know there are five distinct stages of tooth decay? And, that in the first stage of decay, you can actually take steps to reverse the progression of the disease? Indeed, it’s true. In the first stage of decay, whether you’re a child or an adult, the application of fluoride via fluoride treatments, your toothpaste and even the local water supply can stop a cavity from penetrating through the enamel and reaching its second stage. Even the saliva in your mouth and the foods you eat help to re-mineralize a tooth in jeopardy. But that’s just the first stage! What about the rest?
Preventing the Progression of Tooth Decay
Understanding how a cavity progresses can assist you in preventing each successive stage from occurring in your children. There’s always a lot going on in that little mouth!
-
Stage One: White Spots
In stage one, the tooth begins to show signs of strain from the attack of sugars and acids, and white spots will begin to materialize just below the surface of the enamel. These white spots are representative of the demineralization of the tooth and can be easy to miss because they’re likely to occur on your child’s molars. A dental exam, of course, is designed to catch such cavities! Can you see why regular visits to the dentist are recommended? As mentioned previously, at this stage, the cavity can be repaired without the need to excavate the tooth.
-
Stage Two: Enamel Decay
Stage two marks the beginning of the end for the surface enamel that is being attacked. Initially, the tooth erodes from the underside outward, so the outer enamel will still be intact for the first half of this second stage. Once the cavity breaks through the surface of the enamel, there is no turning back, and your child will need to have the cavity corrected with a filling.
-
Stage Three: Dentin Decay
If a cavity in your child’s mouth were to progress beyond stage two without you knowing, you’d tend become aware of it when it started to hit stage three because it would probably start to cause some pain. At this level, the cavity begins to eat away at the second level of tooth material that lies beneath the enamel: the dentin. A filling can still be used to stop the onslaught of bacteria assaulting the tooth in order to prevent the cavity from reaching the tooth’s most critical component: the pulp.
-
Stage Four: Involvement of The Pulp
Once the cavity reaches the pulp, it’s going to hurt. A lot. So if you’ve unfortunately missed all the signs to this point, a screaming child or moaning teenager will certainly let you know there is a big problem. Stage four is serious, and a root canal is the only option of treatment at this stage, save for a complete extraction.
-
Stage Five: Abscess Formation
In the fifth and final stage of a cavity, the infection has reached the tip of the root and exited the tip of the tooth’s structure. This in turn infects the surrounding tissues and possibly the bone structure. Swelling would be commonplace and pain severe. In children (as well as adults) an abscess can be fatal if not dealt with immediately. Root canal or extraction would be the order of the day should decay reach this stage.
As you can see, cavities don’t happen overnight. In the early stages, regular visits can stall and reverse the progression of these dastardly little devils, so it really does pay to visit the dentist at pre-selected intervals. You can keep your kids far from stage five their whole lives, and if a little bit of prodding to get them to the dentist accomplishes that, you can rest easy despite the griping.
Tempormandibular Joint Disorders
Temporomandibular Joint Disorders (TMJ or TMD)
The temporomandibular joint attaching the jawbone to the skull is the most used in the human body. It allows the mouth to open and close for eating, speaking, chewing, breathing, and laughing. It can move up, down, back, forth, and side to side. This nearly constant use of an extremely complex network of muscles and ligaments surrounding a ball and socket joint can lead to painful complications that affect its movement and function. These issues are collectively labeled as temporomandibular joint disorders, or TMD, although some people refer to them as TMJ, which is the name of the joint.
Symptoms of TMD
When the temporomandibular joint becomes inflamed or irritated, it can trigger various symptoms that limit movement and cause joint damage. These symptoms can include:
- Teeth clenching or grinding (this may be a symptom or a cause)
- Morning jaw pain or stiffness
- Difficulty opening or closing your mouth
- Pain when chewing
- Clicking or popping of the jaw
- Misaligned bite
- Difficulty tearing food
- Pain in the back teeth that is not wisdom teeth
- Migraines or chronic morning headaches
- Chronic pain around the eyes or cheekbones
- Chronic earaches
- Worn-down teeth on one side
- Ringing in the ears (tinnitus)
- Difficulty sleeping
- A jaw that feels like it is “stuck” or “locked” in place
These symptoms, left untreated, can worsen and lead to anxiety, depression, broken teeth, and other complications. If you have any of the above symptoms for more than a few weeks, you should see a dentist for proper evaluation of the joint.
Diagnosis of TMJ Disorder
A complete evaluation by your dentist is necessary to treat TMJ Disorder properly. This comprehensive process includes checking your jaw joints and muscles for tenderness, popping or clicking, and range of motion. X-rays are usually taken and reviewed, and a digital image of your teeth may be taken to determine how your teeth fit together. This thorough evaluation ensures that the causes of your TMJ disorder are accurately identified.
Temporary Relief of TMJ Pain
Finding lasting relief from TMJ usually requires treatment by a dentist or TMJ specialist. However, you can take steps to relieve pain or stiffness temporarily. If your TMJ is bothering you, try these solutions until you can be seen by a dentist specializing in TMJ Disorders:
- Gently massage the joint.
- Take Acetaminophen or Ibuprofen to reduce inflammation.
- Apply warm, moist compresses to the sides of the face for 15-20 minutes, repeating as needed.
- If warm compresses do not help, try ice packs for 15-20 minutes at a time with 15-20 minutes in between.
- Stretch the joint by opening and closing the mouth slowly several times.
- Avoid gum, caramels, or anything that requires significant chewing.
- Sleep on your back to avoid shifting your jaw out of alignment.
Treatment of Temporomandibular Joint Disorders
Treating TMJ Disorder can be difficult because of the complexity of the issue. There may be more than one underlying cause that needs addressing. Among the options for treatment are:
- Physical Therapy: To improve range of motion, reduce pain, and loosen tight muscles. This is an ongoing process that requires dedication.
- Steroid Injections: Steroid injections can reduce inflammation and pain for several weeks.
- Botox Injections: These injections can temporarily relax or paralyze specific muscles, and block pain signals to the brain for 3-4 months.
- Oral Appliances: Dentists can create customized oral splints to address the cause of your TMJ. Depending on the individual’s needs, the oral appliance may prevent teeth grinding, stabilize the jaw, or prevent the jaw front from sliding too far forward or backward while sleeping.
- Surgery: Orthognathic (jaw) surgery is a last resort after all other options have failed to bring relief. This invasive surgery repositions or replaces part of the jaw and requires months of physical therapy after a lengthy healing process. However, the results last a lifetime.
If you have symptoms of temporomandibular joint syndrome, it’s crucial to contact your dentist as soon as possible. Early intervention makes treatment simpler and more effective.
When Will Baby's Teeth Arrive A Guide
Understanding Teething in Babies
Before your little one can talk, it’s a guessing game to figure out what may be causing them pain or discomfort. But if they’re drooling, nibbling on hands or toys, or seem extra irritable for no reason, chances are they’re teething. Just peek in that adorable little mouth and you might be able to see some teeth sticking through those gums!
Fortunately for your baby, teeth don’t all erupt at once. Ouch! Instead, they typically follow a predictable pattern of eruption.
So when can you expect them? Read below!
Baby’s teeth, in order of appearance
1. Two bottom teeth (central incisors) – erupt between 6-10 months
2. Two top teeth (central incisors) – erupt between 8-12 months
3. Top two lateral incisors (right next to two front teeth) – erupt between 9-13 months
4. Bottom two lateral incisors (right next to bottom two teeth) – erupt between 10-16 months
5. First molars (on top) – erupt between 13-19 months
6. First molars (on bottom) – erupt between 14-18 months
7. Top canines (cuspids) – erupt between 16-22 months
8. Bottom canines (cuspids) – erupt between 17-23 months
9. Second molars (on bottom) – erupt between 23-31 months
10. Second molars (on top) – erupt between 25-33 months
*For a visual, click here.
Remember, this is just a guide. Your baby may be teething on an earlier or later schedule, and that’s okay!
In fact, your babe might be teething months in advance of the appearance of a tooth. Just keep those drool bibs handy, with plenty of safe toys to chew on, and maybe a couple of other tricks up your sleeve (ask your pediatrician what they recommend), and you and your little one will get through this season just fine.
The Perfect Road Map To Oral Health

On July 3rd, 1806, two years into their journey to chart the unchartered West of America, pioneer explorers Meriwether Lewis and William Clark reached a challenge of epic proportion – the Rocky Mountains. What next, they wondered? Without a map, they were forced to do what explorers do – explore, and hope for the best. So, that got us thinking. Wouldn’t it be nice to have a handy map you could use to chart your own dental health? With that in mind, and in honor of our “Dog Days of Summer” explorers, here are a few mile markers you can use to stay on top of your health today, next year, and for years to come!
18-25 years old
This is a time where work, college, and sometimes marriage start to get in the way of our parental-guided dental care regimens. It’s also a time when even as college students, we tend to find money for the things we “want” instead of the things we “need.” Given that we’re generally healthy at this time in our lives, there isn’t too much we have to worry about when we visit the dentist. Yet here are a few conversations you might want to have with the doctor when you come in for your periodic cleaning:
26-39 years old
These are the years where decades of wear-and-tear start to catch up with you. They’re also bridge years for having kids, and you’ll feel as though life is pulling you in a million directions. Ignoring the dentist during this timeframe is risky. Here’s how you can stay ahead of the game:
40-65 years old
With maintenance and repair top of mind, you’ll want to start to educate yourself on the sort of procedures that will help you keep your healthy teeth, and strengthen or replace those that are weak. Consider:
65+ years old
At this age, you’ll need to consider a multi-disciplined approach to your dental care. Aside from aging teeth, you may also have other health concerns that disrupt your typically healthy mouth. Some things to consider are:
Staying on top of your oral health isn’t as hard as you think, and if you keep this schedule of events to watch out for handy, you’ll be ahead of most of your neighbors when it comes to a healthy mouth and body. Come to think of it … why not share it with them as well? They’ll thank you for the help!
How Harmful Is ThumbSucking to My Baby's Teeth
Thumb-Sucking in Babies

Thumb-sucking is extremely common in babies – and very cute! Babies have very few items in their self-soothing arsenal, but when all else fails, a good ol’ thumb will do the trick to calm them down. For some babies, thumb-sucking comes and goes. For others, the habit lasts well beyond when it should. What’s the harm exactly? And when do we need ensure our kiddos stop?
Why do babies suck their thumb?
Babies are born with the need to suck; in fact, sucking is a reflex and baby will suck anything that hits their palate. This reflex ensures baby sucks and swallows the good stuff – breastmilk or formula – which is their only form of nutrition until they’re ready for solids. The act of sucking is innately soothing for a baby. When babies are tired or stressed, you’ll often find that milk, a pacifier, or a thumb will do the trick to calm them down.
What’s the harm in it?
A baby sucking her thumb needn’t worry about any future orthodontic concerns. But thumb-sucking beyond the baby years can affect how a child’s teeth and palate are shaped. That is – when a child’s permanent teeth are coming in, usually after the age of five, continued thumb-sucking can cause teeth to be misaligned. A child’s front teeth may protrude out and his palate may be misshapen due to constant upward pressure. Due to the teeth being misaligned, your child may also have speech problems. The severity of dental and speech problems will depend on how vigorously and frequently your child sucks their thumb.
How do I get my child to stop thumb-sucking?
The sooner you help your child curb the habit, the better. But if your child is still sucking her thumb after the age of five, you’ll want to put in a more concentrated effort (without creating any power struggles). Try some of these tips from the University of Michigan Department of Medicine, or ask your dentist or pediatrician for other ideas.
Sip and Snack All Day? Risk Decay!
The Magic of Reversing Tooth Decay Fun Science
Introduction
Okay, so here’s a neat idea. Did you know that even though a cavity may start to form in your mouth, there are ways to reverse that decay? Pretty cool, huh?! It’s possible. And, it’s neat as heck. We’ll tell you about it. There are also these little cells called odontoblasts (doesn’t that sound like it’s something from Star Wars!?) … yeah, and they lay down this layer of protection against approaching cavities like it’s a battle, and … Wait! Grab the kids so they can learn too!
Your teeth are pretty amazing. They’re also exceedingly good at “recognizing” their importance in your life. Teeth allow are critical for sustenance, to the structure of your face, and in the ability to interact with others with a smile. It’s no wonder then, your pearly whites like to take care of themselves – all the way to the cellular level … to the Odontoblasts!
A Look at Odontoblasts
Odontoblasts are columnar cells that live in our teeth along the border between the pulp and the dentin. One of their main roles is to continually secrete fresh dentin to allow our teeth to remain strong and healthy. Remember, your teeth are living sensory organs, so these little cells are at it all the time. They’re also very proactive when a cavity begins to encroach on its territory.
When a cavity progresses to the degree that it threatens the integrity of the pulpal chamber (which would require root canal treatment), Odontoblasts feverishly get to work laying down additional layers of dentin to protect the pulpal chamber. To get a feel for what this might look like, imagine a cavity driving down straight from the top of your tooth, aiming straight for the pulpal chamber in the middle of your tooth. The Odontoblasts (along with nearby stem cells), recognizing this impending attack essentially throw up their “shields” (dentin), in an effort to stay safe. This reduces the overall height of the pulpal chamber ever so minimally, but enough to protect the chamber. This is one good reason why you don’t want to ignore tooth pain … jeez, those little Odontoblasts are trying to protect you for all their worth … help them out and see the dentist!
What about Reversing Tooth Decay?
Tooth decay is progressive. It can also be reversed, IF you catch it early enough. And, in this scenario your two best allies are your dentist, and fluoride.
Let’s take a quick look at fluoride. This mineral’s role when it comes to your teeth, is teaming up with calcium and phosphate to strengthen the enamel through the process of remineralization. When fluoride is added to the calcium and phosphate ions that exist in our saliva, and that we also get from food, the three combine to form a mineral known as fluorapitite. This mineral is then transported by our saliva into the “pores” of our teeth, effectively making our enamel harder than it would be by nature. Why is this important? Because tooth decay happens slowly, and in its first stage, the damage it’s beginning to inflict can be stopped or reversed with the assistance of fluorapitite.
In this first stage of a cavity’s development, a cavity appear on the surface of the enamel as a white spot. They’re often visible to a dentist, and will show up on an X-ray. Again, they don’t show up overnight, so two visits a year to the dentist is your best course of action to catch these things early. After all, you don’t want those poor Ondontoblasts to have to go through all that stress just to save you from yourself, do ya’?
Odontoblasts and Fluorapitite. Your secret weapons in dental health. Oh, and your dentist as well! How could we forget?!
My Child is Missing a Tooth What are Our Options
My Child is Missing a Tooth. What are Our Options?

When a child is missing a permanent tooth due to congenital reasons, or loses one due to trauma, the desire to fill that space (particularly if you’re dealing with a teenager) can be pressing. Rest assured, there are several options you can pursue to help improve the functionality of their bite and add to the overall cosmetic appearance of their smile. Some options, however, may not be immediately available – even for teens nearing graduation. Let’s look at why that might be the case, and what your options are.
Orthodontics
There are several scenarios in which orthodontics can be used as a solution. One is when orthodontics helps create a space in the area where a tooth should have arrived, but didn’t, and is now occupied by another tooth that filled in the gap. Doing so would ideally create room for an implant. The second option would be to close a space left by a missing tooth by guiding others into position to close that gap. In this example, tooth shaping is sometimes employed to properly fit and mimic the look of the type of tooth that would naturally be in that spot.
Implant
While an implant would seem to be the absolute best solution for missing teeth because of its strength, durability and cosmetic appeal, implants are only viable after a child has concluded the growth phase of adolescence. Doctors can determine if a child has stopped growing by performing a series of 360 degree cranial X-rays known as cephalometric scans. You may read that once teens have reached a certain age, it’s safe to assume they have stopped growing and can be fitted with an implant, but because each of our children is different, the only way to be certain is to work with your dentist to determine the right time for placement.
Removable Bridge
Another common approach is to employ a removable bridge. Such a bridge is technically considered a denture, since it is removable, but also a bridge because it bridges the gap between any number of missing teeth. These partials provide stability for the bite and a reasonable amount of cosmetic appeal. Because they’re like retainers used after the removal of braces, some can find them to be uncomfortable at first, but in time, they’re easy to get used to. Kids of all ages tend to enjoy pulling these out and scaring the heck out of friends. “Look what I can do!”
Traditional Bridge
Like a partial, a traditional bridge serves the same function of bridging any gaps between teeth, but unlike partials, a traditional bridge is fixed. In other words, it’s not removable, and is adhered directly to the surface of the teeth opposing the gap. Fixed bridges are sometimes preferred over removable bridges, but they can be more of a challenge to clean and do require reducing certain healthy portions of adjacent teeth.
Composite Bridgework
A composite bridge is a compromise between a fixed bridge and a partial. With a composite bridge, the dentist would shape a “replacement” tooth with bonding material and adhere it to the surfaces of the adjacent teeth without having to remove healthy tooth material from those adjacent teeth. It could also be removed by the dentist at a later time with relative ease should an implant or other solution be preferred. It has some of the same cleaning challenges as a fixed bridge, however, so proper oral care is essential. Missing a tooth really isn’t the end of the world and, of course, there are solutions your dentist can provide to help fill in that gap.
Types of Dental Implants
Types of Dental Implants
Dental implants are often an ideal replacement for missing teeth. They can last 20–30 years or longer and usually last a lifetime. They offer many advantages, including supporting your facial structure, restoring your ability to eat any foods you like, and preserving jawbone health. However, many dental implant options are available; understanding the different types of dental implants can help you choose the right type for your dental restoration.
Single Dental Implant
When a single tooth is missing, a single implant tooth can be placed without disturbing the teeth on either side. The implant screw is surgically placed in the jawbone, where it fuses with the jawbone, creating a stable base for the restoration that is attached.
Multiple Implants
When you are missing several teeth not in a row, you can have them individually replaced, each with its implant and attached crown. This allows your dentist or oral surgeon to place an implant for each missing tooth and attach an individual crown to each one.
Implant-Supported Bridge
If you have several missing teeth but would like to use a bridge rather than individual restorations, a bridge containing all the replacement teeth can be supported by a few carefully placed implants.
Full-Arch Dental Implants
When you are missing all the teeth in the upper or lower jaw, a full arch of replacement teeth can be fastened permanently to between four and eight or more implants that are precisely placed in the jawbone to take advantage of the widest and strongest areas of the jawbone.
All-On-X
All-On-X is a generic term for any full-arch dental implants supported on a specific number of implants, usually four or six. The most common forms of this are the All-On-4® and All-On-6® dental implant processes.
Implant-Supported Dentures
These are dentures that are attached to implants placed in the jawbone. Fixed implant-supported dentures are not removable but suspended just above the gums so you can clean beneath the denture. Removable implant-supported dentures snap into place on posts or bars attached to the implants in the jawbone. These can be removed when you are sleeping and for cleaning.
Zygomatic Implants
Individuals who do not have enough bone mass in the upper jawbone to support dental implants may have to get zygomatic implants. Zygomatic implants use longer implant posts that are secured in the cheekbones rather than the jawbone, taking advantage of the significantly denser, stronger bone found there. Patients who do not have sufficient jawbone for traditional implants are usually successful with zygomatic implants.
Your dentist can help you determine which type of dental implant is best for you.
Tooth Decay
Tooth Decay
Tooth Decay is a result of bacteria in the mouth that makes acids that eat away at the tooth. When sugar and starches are consumed on a regular basis and plaque is left on the teeth, it produces acids and destroys tooth enamel over a period of time. Tooth decay will often lead to cavities if left untreated.
Treatment
Most tooth decay can be treated by using fluoride, a filling, or, in more extreme cases, through a root canal or a crown.
Prevention
You can prevent tooth decay by regularly brushing and flossing your teeth, regularly scheduling hygiene checkups with your dentist, and limiting foods that are high in sugar.
11 Tips That Can Help Your Child Prevent Cavities
11 Tips That Can Help Your Child Prevent Cavities

There’s nothing worse than subjecting your child to the whir of a dentist’s drill because simple oral hygiene habits were not followed.
Sure, kids hate flossing as much as adults, but if we’re successful at instilling good behavior early on in life, those habits will provide them with a healthy mouth that will keep them smiling indefinitely.
“Ignore your teeth and they’ll go away,” the old saying goes. Protecting your child’s teeth from cavities can be as simple as following a few simple recommendations.
Here are 11 easy things you can do to keep cavities from taking root in your child’s mouth.
1. Regular brushing and flossing:
Brush at least twice a day, floss at least once a day.
2. Don’t share your food and drink:
Cavities can actually be contagious! Because the bacteria that causes them can be passed from one user to the next, it’s best to avoid sharing foods and drink with children.
3. Visit to the dentist:
Most dentists recommend you should bring your child to a dentist after their first tooth arrives. Then, thereafter, based on the recommendation of your dentist.
4. Avoid frequent snacking:
Constant snacking, particularly on sweets, provides the perfect environment for cavity-inducing bacteria to do their work.
Limit snacking to healthy foods, and if your children can brush, or use water as a mouthwash after snacking, that’s even better.
5. Eat crisp, water-dense fruit:
Fruits high in water help keep your child’s mouth hydrated, particularly useful during a lunchbox meal.
6. Avoid additional sugar:
This is good for the body as well, and common sense when it comes to teeth. Soda is a big no-no, of course.
7. Consider dental sealants:
Your dentist can place a protective sealant on your child’s teeth to prevent decay. The process is simple and can save future headaches.
8. Drink a lot of water:
Water should be the beverage of choice. Bottled water is okay, but fluoridated tap water is best. Use a filter if you are concerned about the quality of your local tap water.
9. Minimize juice beverages:
It’s best to drink these in moderation. Juice can be acidic and sweet – two things that are not so good for our teeth.
10. Avoid sticky foods:
Items like fruit leathers, cookies and candies aren’t good choices for healthy teeth any day of the week.
11. Consider cheeses and nut butters:
Nuts and cheese have ingredients that help remineralize our teeth, and can be good additions to a lunchbox.
If you have a child with allergies, soy nut butter might possibly be an option. However, always be sure to check with your allergist first to be certain if soy nut butter is safe for your child to consume.
Questions About Premedicating with Antibiotics We Have Answers

If you’ve been prescribed antibiotics in conjunction with an upcoming dental procedure, you might have a list of questions for your dentist about why. Any time you take antibiotics, it’s important to understand both why you’re taking them and how to take them.
Antibiotics are a wonderful tool in modern medicine to prevent and cure bacterial infections. They have saved countless lives. But the overuse (and misuse — when not taken properly) of antibiotics has created antibiotic-resistant strains of bacteria. This means that you could become infected with a form of bacteria that can’t be treated — and that is a scary thought. For that reason, it’s important to use them sparingly and only when necessary.
Let’s run through the important facts …
Why do dentists prescribe antibiotics (premedication) for dental procedures?
Antibiotics are prescribed alongside dental procedures to prevent bacteremia — a condition in which bacteria enter the bloodstream and spread infection to different parts of the body.
Who requires premedication?
Your dentist will take your whole medical history into account to determine if you require premedication. Make sure they are aware of any and all medications you are currently taking or have taken recently. For instance, if you’ve recently taken antibiotics for strep throat, it’s important that your dentist know this. That way they can prescribe a different type of antibiotic. Your dentist may also need to consult with other physicians you see. This might take some extra time but is worth it!
You might need to premedicate if:
- You have certain heart conditions, such as a heart valve replacement, a history of infective endocarditis, a heart transplant that developed valvulopathy, any unrepaired congenital cyanotic heart defect, or any corrected heart defects with residual defects
- You are immunocompromised by an autoimmune disorder or cancer
In the past, premedication was recommended for heart murmur, mitral valve prolapse, and artificial joint replacements, but current guidelines exclude these conditions.
How does premedication work?
Typically, your dentist will write you a prescription. You will pick it up from your pharmacy and take it 30 minutes prior to your appointment. If you have trouble taking pills orally, your dentist may administer antibiotics while you’re in the chair (via intramuscular injection or intravenously).
Note: it is extremely important to take your antibiotics exactly as they are prescribed. This helps prevent drug-resistant bacteria from developing.
What happens if you forget to premedicate?
Let your dentist know if you have forgotten to premedicate. In most instances, you may still take your antibiotics within two hours of the procedure.
Are there any potential side effects of premedication?
Yes. Any medication has the potential to produce side effects. These could include nausea, upset stomach, allergic reactions, and others. However, there are also risks to not premedicating, including bacteremia and sepsis. This is why you have been prescribed premedication.
Any other questions?
Ask your dental team! If you are hesitant about any part of your health plan, it’s best to speak up and gain clarity!
Your dentist should be up to date on current guidelines set in place by the American Dental Association and the American Heart Association, and will know the ins and outs of your individual situation (as long as you’ve told them everything!). Best of luck!
Does My Child Need a Mouthguard for Sports

A six-year-old missing their two front teeth can be quite the cause for celebration
Just think of all the tooth fairy visits and all relatives marveling at the new, hip look. Now if it’s a teenager without those teeth, well that’s a different story with much less celebration. And such tooth loss happens all the time – particularly if your child participates in sports. In fact, the American Dental Association suggests that athletes are 60 times more likely to experience harm to their teeth if they’re not wearing a properly fitting mouthguard.
Why Your Child Needs A Mouthguard
If your child is active in sports – even the backyard variety – please consider investing in one. The American Dental Association estimates that “a full third of all dental injuries are sports related … and that the use of a mouthguard can prevent more than 200,000 oral injuries to the mouth each year”. The risks of playing sports without protection aren’t just related to teeth loss: a harsh impact to the jaw can even affect the growth of facial features or cause a concussion that could have otherwise been avoided.
When choosing a mouthguard, it’s important to remember that custom-made guards are far superior to the “boil and bite” variety at local sporting goods stores. They are designed using a process similar to that used when making an orthodontic retainer, and guarantee a perfect fit to your child’s mouth. The fit is the most important aspect of a protective mouthguard. Variations in the preparation and specifications of custom guards depend on the type of sport your child plays, as well as their age and overall dental health. On the fun side of things, guards can also be made to match your child’s school colors, or can feature the logo of their favorite professional team.
When There’s Convincing to Do
At first, you may find that your child objects to the idea of wearing a mouthguard, much in the same manner as when you suggested they wear a helmet while cycling. This is natural, and if you experience kick-back, it might help to show them pictures of their sports heroes wearing guards. After all, mouthguards are commonplace in professional sports, and there’s no reason your child wouldn’t want to imitate more than just their favorite player’s moves. If you’re still wondering whether investing in a mouthguard is worth it, you’ll be pleased to know that these dental appliances are rather affordable, and can even sometimes be covered by your insurance. You will also sleep better at night without the prospect of huge dental surgery bills – and knowing your child won’t going through school with a 1970’s hockey-star smile.
Are My Gums Receding And Why
Understanding Gum Recession
Progressive change can be difficult to notice, especially when it occurs to us and not someone else. Changes occurring along our gum line certainly fall into this category, and since recession is measured in millimeters it’s especially easy to miss.
So, how much gum erosion is normal, and what causes it? Let’s take a look.
Is Gum Recession Normal?
Gum recession is often considered a normal part of aging. Even the expression “long in the tooth” stems from our gum line receding and exposing more of our teeth as we age.
However, there is nothing normal about gum recession. Luckily, for most of us it can be prevented.
Rather than keep things as they are, embracing gum recession as the well-paid price of wisdom, be vigilant against gum erosion! Though there are a host of factors that contribute to the erosion of your gumline, a vast majority are preventable.
The Biggest Offenders
- Clenching or grinding your teeth
- Over-vigorous, or improper brushing
- Aggressive flossing
- Exposure to acids in sports and energy drinks
- Tobacco use
- The frequent use of whitening products
All the above causes of gum loss can be prevented.
All of them.
If you grind your teeth at night, wear a mouth guard.
If you brush as though you’re sanding down the statue of David, learn proper technique from your dentist, or from a video online.
Bleeding a lot when flossing? You’re not slicing cheese – go easy, there, friend!
If you smoke, drink too many energy drinks, or chew tobacco, cut back, or stop altogether. None of that stuff is good for you in any way imaginable.
And lastly, if you’re trying to look like a movie star by abusing whitening strips, you can stop now. Your teeth have got to be super-white already!
Be Proactive
What’s next? How can you tell if your gums are receding faster than the Amazon rainforest?
Well, the most proactive step is to visit your dentist. In fact, if you’re going regularly, your dentist has been monitoring the recession for some years now.
If you’ve ever noticed your dentist poking around in your mouth, all while reciting numbers to the hygienist, they’re probably doing two things: measuring the recession of your gums, and gauging the depths of your gum pockets. Both speak to the health of your gum line.
So, the next time you hear your dentist reading off what seem like lottery number, just ask about the health of your gums … your dentist will be happy to keep you in the loop.
The first sign of gum recession is usually tooth sensitivity, so be on the lookout. Reduce, or eliminate the above discussed habits, and ask your dentist how you’re doing in terms of taking care of your gums.
With a little bit of knowledge and proactive behavior, no one will ever say you’re long in the tooth. And, that’s a good thing!
Dental XRays Are They Safe and Necessary
Dental X-Rays: Are They Safe and Necessary?
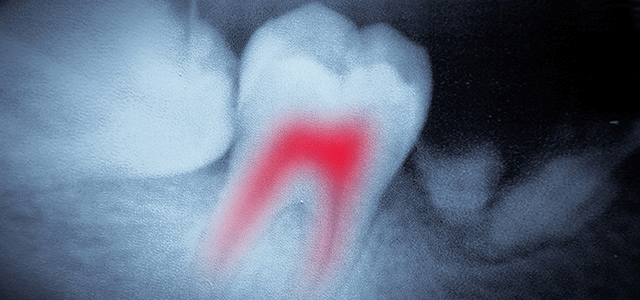 Dentists and hygienists are often asked about the safety and necessity of X-rays. This is a great question – with answers that differ from patient to patient.
Dentists and hygienists are often asked about the safety and necessity of X-rays. This is a great question – with answers that differ from patient to patient.
So let’s examine it a bit further. You may be surprised to learn just how safe today’s X-rays are, and which audience asks this question even more so than patients.
X-ray Safety Is Always Being Tested
So, who asks this question more often than patients? Would you believe, dentists? That’s right!
Together with the FDA (Food & Drug Administration), the American Dental Association (ADA) routinely asks this question, and revises its guidelines when advances in science and technology provide new methods to reduce exposure.
In fact, thanks to faster film speeds, digital X-rays, and the use of protective aprons and thyroid collars, the X-ray of today is far superior to those of even just a decade ago.
Below are the general guidelines the ADA and FDA recommend for adults. It’s important to remember that because all dental care is patient-specific, these guidelines are to be used to accompany the professional opinion of your dentist. Only your dentist has knowledge of your health history and vulnerability to oral disease, and is in the best position to make such recommendations.
New Patients
Full X-rays are generally suggested for new patients to provide your dentist with a full history of your prior oral care and current needs.
Continuing Care Patient with, or at increased risk for cavities
One set of X-rays every 6-18 months.
Continuing Care Patient with no clinical cavities and not at increased risk for cavities
One set of X-rays every 24-36 months.
Continuing Care Patient with periodontal disease
Dependent upon the professional judgment of your dentist.
New and Continuing Care Patients being monitored for dental/skeletal relationships
Dependent upon the professional judgement of your dentist.
Patients with, but not limited to, proposed or existing implants and root canals
Dependent upon the professional judgement of your dentist.
Do you want to read ADA’s complete guidelines? The full report can be found here.
Diabetes And Dental Health

Introduction to Diabetes and Its Impact on Dental Health
25.8 million children and adults in the United States – 8.3% of the population – have diabetes. And not too far behind those 25.8 million are the estimated 79 million Americans with prediabetes. What’s worse, the increasing prevalence of Type II diabetes has become so staggering, the International Diabetes Foundation has begun to denote Diabetes as “The Global Burden.”
Diabetes is a serious illness, and its complications are manifold. Most know of its impact on circulation, visual acuity, and heart and kidney function. Many aren’t aware, however, of its deleterious effect on gum tissue. If you’re prediabetic, have diabetes or have a loved one with the disease, you’ll want to learn more about how to ward off this commonly unknown side effect of the disease.
Diabetes is a disease with tentacles. It touches and degrades so many aspects of a person’s physical health. Vigilance is needed, particularly with regard to its role in a healthy mouth, because having diabetes can not only lead to oral disease, but the presence of oral disease can also aggravate diabetes. When it comes to diabetes and the mouth, it is unfortunately, as the scientific community calls it, a two-way street.
What are some of the Oral Health complications of Diabetes?
- Tooth Decay: Occasionally, an observant dentist who notices a high instance of cavities in an otherwise healthy mouth is the first to suggest a patient be tested for diabetes. This is because uncontrolled diabetes results in higher levels of salivary glucose. When coupled with a diabetic’s diminished salivary production, the mouth tends to bathe in an environment ripe for tooth decay, and these parallels are markers that get a dentists’ attention. If you’re already diabetic, you’ll want to keep your dentist informed of your disease and its current state so they can always be on the lookout for related problems in your mouth.
- Gingivitis and Periodontal Disease: Because diabetes lowers the body’s ability to fight infection, people with the disease are more likely to encounter bouts with gingivitis and periodontitis. Both gingivitis and periodontitis are bacterial gum infections, with gingivitis being the less advanced version of the two. Having either condition, though, requires diligent care because of a diabetic’s inability to fight these infections properly. Diabetics have the added burden of contending with rising sugar levels caused by the body’s reaction to stress and infection. The resulting see-saw effect can be quite difficult to manage, to say the least.
- Fungal Infections: Also related to the body’s inability to fight infection, diabetics are likely to experience a greater incidence of oral fungal infections. Thrush, which can be common in infancy as a baby, develops their immune system is often seen in diabetic patients as well.
- Loss of Taste: In the far-reaching realm of diabetes complications, losing your ability to taste certainly ranks among the most unpopular. Here, nerve damage is the culprit, as untreated or uncontrolled diabetes can cut off nerve transmissions to the brain from the taste buds, thus impairing or completely removing one’s ability to taste.
Diabetes is a serious illness. If you already have the disease, it can be controlled by following the advice of your doctor and your dentist. Be sure to make all of your health care team members aware of your disease so you can best stay on top of it.
Proactive Planing and Scaling Can Prevent Advanced Gum Disease
Proactive Planing and Scaling Can Prevent Advanced Gum Disease
 Contrary to popular belief, gum disease does not discriminate based on age. Both adults and children can find themselves battling bleeding gums and gum recession – both signs of gingivitis, and the more serious advancement of the disease, early onset periodontitis. To prevent this bacterial infection which can eventually cause tooth and bone loss, your child’s dentist may recommend a proactive approach that includes a more thorough type of cleaning known as root planing and scaling.
Contrary to popular belief, gum disease does not discriminate based on age. Both adults and children can find themselves battling bleeding gums and gum recession – both signs of gingivitis, and the more serious advancement of the disease, early onset periodontitis. To prevent this bacterial infection which can eventually cause tooth and bone loss, your child’s dentist may recommend a proactive approach that includes a more thorough type of cleaning known as root planing and scaling.
Similar the typical dental cleaning which takes place above the gumline on the tooth’s enamel, root planing and scaling is performed on the cementum of the tooth (the outer layer of the tooth’s root that exists below the gumline. This process is recommended if “early active” periodontitis is witnessed in combination with tartar buildup, and if any portion of the gumline has noticeably pulled away from the tooth.
You should remain particularly attuned to these symptoms if you are the parent of children progressing through puberty. Reason being, the rush of hormones that plagues both boys and girls as they mature not only affects their voices, height and physical development, but surprisingly, the environment within their mouths as well. The result of this increased level of hormonal activity can result in gingivitis, and girls are even more likely to suffer from complications than boys, because of the specific reactions of estrogen and progesterone toxins within the mouth. So, as a parent, it’s important to be aware of these changes that might be presenting themselves in the mouth of your children.
The root planing and scaling procedure itself first involves the application of an anesthetic to numb the affected areas, and an antiseptic to lessen the volume of live bacteria in the mouth. Next, using a sharp hand tool called a curette, your child’s dentist would scrape off (or, “scale”) the hardened tartar deposits on the root of the tooth in an upward motion. An electric ultrasonic scaler may also be used to break off the deposits from the tooth should the curette not prove as complete a solution. Any deposits left behind by the ultrasonic scaler can be scraped off by hand.
After this, your child’s dentist will then smooth out, (or, “plane”) the root surfaces. Planing is the process whereby a woodworker takes a long roughened edge of a board and makes it smooth by using a “planer.” The same general technique is used here to make the cementum smooth once again, and more equipped to combat plaque buildup in the future.
Because it is effective in eliminating infection, proactive scaling and root planing is often the only treatment needed for early onset periodontal disease and can prevent further complications. If your child is experiencing bleeding, swollen gum tissue, or has any type of discharge from their gums, be sure to have them in for an exam as soon as possible. Treating gingivitis and periodontal disease early and aggressively is a step you’ll most certainly want to take to ensure superior oral health for your child as they enter adulthood.
Thinking about Having A Baby Or Recently Pregnant
Thinking About Having A Baby, Or Recently Pregnant?
 If you’re considering getting pregnant, or are already expecting, concern over the status of your teeth might not be at the top of your list as of late. However, if you’re early enough into a pregnancy, or planning one, you should actually schedule an appointment to see your dentist sooner rather than later. If your stack of pregnancy-related reading material hasn’t already included a chapter on oral health, let us help by providing you the short version as to why you should make that appointment soon.
If you’re considering getting pregnant, or are already expecting, concern over the status of your teeth might not be at the top of your list as of late. However, if you’re early enough into a pregnancy, or planning one, you should actually schedule an appointment to see your dentist sooner rather than later. If your stack of pregnancy-related reading material hasn’t already included a chapter on oral health, let us help by providing you the short version as to why you should make that appointment soon.
Good oral health is the key to good overall health. You know that already. And during pregnancy, your oral health contributes to the health of your baby. Here are a few things to be mindful of in the coming months as you plan your pregnancy:
- Visit your dentist early: Generally speaking, dental work can be safely performed through the first half of the third trimester, but earlier is always better – preferably before pregnancy. The American Dental Association has pointed to research linking premature birth and low birth weight to women with periodontitis (gum disease): a sure enough reason to schedule a full check-up early. While this might seem like something you can brush off if you’re not already suffering from gum disease, that wouldn’t be wise. Why? Hormones, and the sneak-attack caused by Pregnancy Gingivitis.
- Pregnancy Gingivitis: Hormones play a pivotal role in a woman’s life, and during pregnancy they’re out in full-force. During pregnancy, this natural rise in hormones causes an increase in blood flow to gum tissue which can cause some women to experience swelling and tenderness in their gums. This increase in blood flow also tends to cause gum tissue to exaggerate the way it reacts to existing plaque in the mouth, and can trigger what is known as “pregnancy gingivitis.” If ignored, gingivitis leads to the aforementioned periodontitis, and a true cause for concern during pregnancy. That’s why it’s so important to see your dentist as early as possible.
- Pregnancy Tumors: While the name might cause you some concern, these benign growths, which frequently appear along the gumline, are more of a nuisance than anything else. Only about 10% of women get them, and typically in the second trimester. Like pregnancy gingivitis, they’re usually the result of increased hormonal activity and improper oral care.
As you can see, your dentist can and should be one of your many allies in the path to motherhood. So see your dentist early, and as often as is suggested during your pregnancy. You’ll be pleased you did, and so will your baby!
Your Child's First Visit to the Dentist
When Should Your Child See the Dentist for the First Time
The arrival of your baby’s first tooth is an exciting time!
No doubt those weeks (or months) of drooling and gnawing on everything must have been leading to something! Now that those teeth have popped, what does a busy parent need to know about caring for them? Well, starting good dental hygiene early is important and visiting the dentist is the next step after that.
When Should You Start Dental Visits?
The American Dental Association and the American Academy of Pediatric Dentistry recommend that your child’s first dental visit occurs within six months after their first tooth erupts, or no later than their first birthday. That might seem a little early, but the fact is that tooth decay can begin as soon as that first little tooth has come through.
Why Should You Start Dental Visits Early?
Getting a head start on dental visits will ensure your little one’s chompers are taken care of. It also familiarizes them with routine dental visits so that they don’t seem so intimidating in the future. If you’re reading this and have yet to take your 3-year-old to the dentist, don’t worry! Simply call and make an appointment now. The sooner you can get in, the better! No parent shame here.
What Happens during the First Dental Visit?
Your child’s first dental visit is likely to involve a simple meet-and-greet, along with a quick check of their teeth. The dentist may do a simple cleaning if the child is willing.
What Comes After the First Visit?
Beyond that, your doctor will recommend routine visits that will involve cleanings, x-rays, fluoride applications, and the option of putting sealants on your child’s teeth. When it comes to the health of your youngster, no question is ever too silly! Ask your dental team about any questions or concerns you may have. Starting early will give your child a great foundation for a lifetime of healthy teeth!
Root Canal Therapy
A root canal is something that we don’t mind as long as it happens to someone else.
Root canal therapy has existed for centuries and actually was first performed in ancient civilizations – although most often only the nobility and the very wealthy were treated.
Root canal treatment is used to save teeth which would otherwise need to be removed.
It is needed when the blood or nerve supply of the tooth (known as the pulp) is infected through decay or injury.
Sometimes, due to trauma or decay the “nerve” inside the tooth dies off (please do not confuse that with your “tooth” being dead, that is simply not true!). Any passing bacteria find this a source of nourishment and proceed to munch on the dead nerve and quickly reproduce. Your body can’t do anything about this infection because along with the nerve dying, the blood supply to the tooth dies off too, so the body can’t send in some antibacterial cells (white blood cells) to attack the bacteria. Eventually, the bacteria start to spill out of the tooth and into the tiny space between the tooth and the jawbone. This starts an abscess, the body reacts to the invasion by pouring in defensive cells, which kill most of the bugs in the area, but still can’t get to the source of the problem, which is in the tooth.
Some indications for a root canal are:
- Pain while biting
- Sensitivity to hot or cold
- Deep decay
- Blunt injury to the tooth
- Infection
What is root canal therapy?
Your dentist will thoroughly examine your tooth to determine if the nerve is infected. The exam includes x-rays and checking the health of the tooth with a pulp tester. Additionally your doctor may also apply cold and heat, tap on the tooth to see if sensitive or press gently on gums around tooth to check for pain.
The treatment can take from one to three visits during which typical treatment involves:
- Making an opening through the crown of the tooth and into the pulp chamber
- Removing the pulp. The root canal is cleaned, enlarged and shaped to a form that can be filled.
- (Optionally) Placing medication into the pulp chamber and root canal to help get rid of any germs and prevent infection.
- Placing a temporary filling in the crown opening to protect the tooth before your next visit. Alternatively, your doctor may leave the tooth open for a few days to drain.
- Filling and sealing the pulp chamber and root canals.
- Removing the temporary filling, followed by cleaning and filling of the pulp chamber.
- And finally, placing a gold or porcelain crown over the tooth.
Periodontal Disease Don't wait until it hurts
Are My Gums Receding And Why
Understanding Gum Recession
Progressive change can be difficult to notice, especially when it occurs to us and not someone else. Changes occurring along our gum line certainly fall into this category, and since recession is measured in millimeters it’s especially easy to miss.
So, how much gum erosion is normal, and what causes it? Let’s take a look.
Is Gum Recession Normal?
Gum recession is often considered a normal part of aging. Even the expression “long in the tooth” stems from our gum line receding and exposing more of our teeth as we age.
However, there is nothing normal about gum recession. Luckily, for most of us it can be prevented.
Rather than keep things as they are, embracing gum recession as the well-paid price of wisdom, be vigilant against gum erosion! Though there are a host of factors that contribute to the erosion of your gumline, a vast majority are preventable.
The Biggest Offenders
- Clenching or grinding your teeth
- Over-vigorous, or improper brushing
- Aggressive flossing
- Exposure to acids in sports and energy drinks
- Tobacco use
- The frequent use of whitening products
All the above causes of gum loss can be prevented.
All of them.
If you grind your teeth at night, wear a mouth guard.
If you brush as though you’re sanding down the statue of David, learn proper technique from your dentist, or from a video online.
Bleeding a lot when flossing? You’re not slicing cheese – go easy, there, friend!
If you smoke, drink too many energy drinks, or chew tobacco, cut back, or stop altogether. None of that stuff is good for you in any way imaginable.
And lastly, if you’re trying to look like a movie star by abusing whitening strips, you can stop now. Your teeth have got to be super-white already!
Be Proactive
What’s next? How can you tell if your gums are receding faster than the Amazon rainforest?
Well, the most proactive step is to visit your dentist. In fact, if you’re going regularly, your dentist has been monitoring the recession for some years now.
If you’ve ever noticed your dentist poking around in your mouth, all while reciting numbers to the hygienist, they’re probably doing two things: measuring the recession of your gums, and gauging the depths of your gum pockets. Both speak to the health of your gum line.
So, the next time you hear your dentist reading off what seem like lottery number, just ask about the health of your gums … your dentist will be happy to keep you in the loop.
The first sign of gum recession is usually tooth sensitivity, so be on the lookout. Reduce, or eliminate the above discussed habits, and ask your dentist how you’re doing in terms of taking care of your gums.
With a little bit of knowledge and proactive behavior, no one will ever say you’re long in the tooth. And, that’s a good thing!
Why Do I Need a Bridge?
Why Do I Need a Bridge?
A dental bridge is a prosthetic device that fills the gap left by missing teeth. It consists of one or more artificial teeth, called pontics, which are held in place by adjacent natural teeth or dental implants. Bridges not only improve the appearance of your smile but also help maintain the structure and function of your teeth and jaw.
Why Do I Need a Dental Bridge?
If you have missing teeth, getting a dental bridge is essential for several reasons:
- Restoring Function and Preventing Shifting: Missing teeth can make it difficult to chew and speak properly. A bridge not only helps restore these functions but also prevents the shifting of neighboring teeth into the space, which can lead to misalignment and bite problems.
- Prevents Shifting: When a tooth is missing, neighboring teeth can shift into the space, leading to misalignment and bite problems.
- Maintains Facial Shape: Your teeth support your facial structure. Missing teeth can cause your face to appear sunken or aged. The lips look thinner and flattened, the chin moves forward and looks more pointed, and your cheeks begin to sag, creating jowls. A dental bridge can reverse these effects, restoring a more youthful and vibrant appearance.
- Enhancing Aesthetics: A dental bridge not only fills the gap in your smile but also significantly improves your appearance, boosting your confidence.
- Prevents Additional Tooth Loss: When teeth shift, or your bite is unbalanced, additional strain can lead to further tooth loss over time. A dental bridge acts as a protective barrier, preventing this potential loss and ensuring the stability of your oral health.
Types of Bridges
Fixed Dental Bridge
The most common type is a fixed bridge, which consists of one or more artificial teeth held in place by crowns cemented onto adjacent natural teeth. This option is durable and provides a natural look and feel.
Implant-Supported Bridge
Dental implants rather than natural teeth anchor an implant-supported bridge. This type of bridge is ideal for patients who are missing multiple teeth and want a long-term, highly stable solution. Because implants integrate with the jawbone, they provide excellent support and help maintain bone density.
Caring for Your Bridge
Proper care is essential to ensure the longevity of your dental bridge:
- Maintain Good Oral Hygiene: Brush twice daily and floss carefully around the bridge to prevent plaque buildup.
- Use a Special Floss or Water Flosser: Since food particles can get trapped beneath the bridge, using a floss threader or water flosser can help keep the area clean.
- Regular Dental Checkups: Routine visits to your dentist are crucial to ensure that your bridge remains in good condition and that surrounding teeth and gums stay healthy.
- Avoid Hard or Sticky Foods: Chewing on hard objects or sticky foods can damage your bridge over time.
A dental bridge is a valuable solution for replacing missing teeth, restoring function, and maintaining oral health. Whether you opt for a fixed or implant-supported bridge, proper care will help ensure long-lasting results. If you’re considering a dental bridge, consult your dentist to determine the best option for your smile.
Why Do I Need a Crown?
Why Do I Need a Crown?
A crown, a dental cap, is a protective shield placed over a damaged or missing tooth. It restores the tooth to its original size, shape, and function, safeguarding it from future damage and enhancing its appearance and oral health.
You may need a crown for a number of reasons. Your dentist may determine you need a crown if:
- A tooth is severely decayed, and there isn’t enough structure remaining for a filling.
- A tooth is severely damaged or broken and must be repaired to function properly.
- You need a bridge to replace missing teeth, which will be supported by a crown placed over healthy teeth.
- You have had a root canal and need the tooth covered to protect the interior of the tooth from reinfection.
- You have a weakened tooth that is at risk of fracturing.
- A fractured tooth needs to be restored.
- A tooth is discolored or misshapen.
- You have a dental implant that needs a restoration.
Why is a Dental Crown Better Than a Tooth Extraction?
If you have a decayed or damaged tooth and your dentist recommends a crown, they want to save your tooth rather than extract it. While you may think that extracting the tooth is simpler and less expensive, there are several reasons why removing a natural tooth should be a last resort. When you remove a tooth without replacing it, a cascade of problems can develop that negatively affect your oral health, including:
- Deterioration of the jawbone
- Collapse of the tooth socket
- Shifting of the remaining teeth, resulting in misalignment
- Difficulty eating and speaking clearly
The Crown Procedure
Getting a crown is a simple, minimally invasive procedure, usually requiring two visits to your dentist.
On your first visit, the tooth is prepared by removing any damage or decay and a portion of the exterior so there is room for the crown. An impression is made of the tooth to be used to create the crown. You will leave wearing a temporary crown over the tooth.
The permanent crown will be ready in about two weeks, and you will return to your dentist. They will remove the temporary and place the permanent crown, carefully checking the fit and smoothing any rough edges. Once your dentist is happy with the fit and function, the crown will be permanently cemented into place.
Your Smile An Owner's Manual
Smile Makeover
Imagine having a bright, perfectly even smile that radiates youth and vitality. With modern cosmetic treatments, it’s easier than you may think.
What is a smile makeover?
A smile makeover is a treatment or combination of treatments that your doctors will custom design to enhance the appearance of your unique smile. For some, a smile makeover may be as simple as a teeth whitening session. Others require a more comprehensive plan that may include porcelain veneers, replacement teeth or a cosmetic gum lift. Before we get started, have your cosmetic dentist first evaluate your unique case to determine which treatment options are right for you.
How long does a smile makeover take?
Modern treatment options make smile makeovers faster than ever before. You can potentially have a fresh, new smile in just two or three visits. The length and depth of treatment will depend on your oral status and the results you desire.
How do I get started?
- Your doctor will discuss your concerns, goals and personal preferences before beginning treatment. With digital imaging technology, we can show you the potential results of your smile makeover before the procedures take place.
- Before beginning the artistic phase of your smile makeover, it is important to first resolve all oral issues. A healthy foundation will ensure that your new smile lasts a lifetime.
You may want to consider a smile makeover if you have:
- Widely spaced teeth
- Crooked or overlapping teeth
- Stained or discolored teeth
- Worn, chipped or broken teeth
- Gummy smiles
- Old dental work
- Mismatched crowns
Dental Sealants What They Are and How They Work
Dental Sealants: What They Are and How They Work
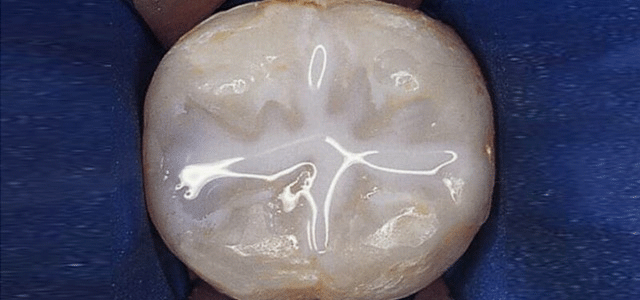
Every dentist wants to ensure children’s teeth are as healthy as possible, and one of the first preventive measures they usually recommend is dental sealants. In fact, The American Academy of Pediatric Dentistry recommends placing dental sealants on the first and second set of permanent molars, which generally come in at 6 and 12 years of age.
But what are dental sealants, how do they work, and why should you choose them for your child?
Why Choose Dental Sealants?
Dental sealants are hardened plastic shields, placed on the chewing, or occlusal, surface of molars and pre-molars, which seal the surface of the tooth.
Sealants work by keeping food and other bacteria-causing material from getting trapped in the tooth and causing decay — which can ultimately lead to cavities.
In one study, kids who received sealant treatment had half the tooth decay of children who brushed regularly but didn’t have sealants.
The Cost and Safety of Dental Sealants
The cost for dental sealants is modest, roughly $30 to $40 per tooth, and is usually covered by dental insurance. The sealants can last anywhere from 5 to 10 years.
Dental sealants were first given approval by the ADA in 1976, and while in the past there had been questions about the use of sealants and if they can be used safely, a new study concludes that sealants are safe if dentists make sure to rinse or wipe away residue after treatment. The journal Pediatrics states that the benefits sealants provide in preventing cavities outweigh any possible risks.
The Benefit of Dental Sealants
Sealants can help prevent food from getting into the places where a child might have difficulty brushing. Without a sealant, it is more likely that your child could develop a cavity in an otherwise unprotected tooth. Cavities require fillings, which run the risk of failure over time.
If you want to give your child’s molars the best protection against potential cavities, dental sealants are a great place to start. Ask your child’s dentist about the possibility of sealants for your child.
Dental Veneers Help to Perfect Smiles
Dental Veneers Help to Perfect Smiles

Everyone wants that Hollywood smile, but not everyone is lucky enough to be born with perfect teeth. Chips, irregular shapes, and discoloration of teeth are not uncommon and can make people hide their smiles or feel uncomfortable.
If your teeth make you self-conscious for any reason, dental veneers may be a solution to consider.
Sometimes called porcelain veneers, or porcelain laminates
veneers are thin shells of tooth-colored material that are adhered to the front surface of your existing teeth to improve their appearance. Your dentist may recommend veneers for one or several of your teeth to correct:
- Worn down teeth
- Fractured teeth
- Discolored teeth
- Chipped or broken teeth
- Misaligned, uneven or irregularly shaped teeth
- Gaps between your teeth
Because veneers don’t usually require as much tooth shaping as crowns do, they are a strong and attractive alternative that preserves as much of the tooth as possible.
Veneers appear very natural and are resistant to staining from coffee, tea or even cigarette smoking. With proper care (which is no different from your standard brushing, flossing, and regular cleanings) veneers can last 5 to 10 years, at which point they can simply be replaced.
Cost and Insurance
The cost of veneers is generally not covered by insurance, as the procedure is considered cosmetic. However, getting that Hollywood smile might just be priceless.
If you would like to learn more about veneers, talk to your dentist at your next scheduled appointment.
Teeth Whitening
Getting a beautiful smile is easier than you think
Do your teeth have more of a yellow tint now? All the coffee, cigarettes or red wine you may have enjoyed took a toll, and that big smile you use to flash is gone. Well, did you know that you can have those stains almost magically erased in the same amount of time it takes to get your haircut, a manicure or even lunch with your friends? Yes, in just a short time you can have a teeth whitening session and bring back that shiny, bright smile again.
Using the latest in tooth whitening technology, a visit to your dental office can make your smile brighter than ever before. Tooth whitening can correct tooth discolorations caused by staining, aging, or even chemical damage to teeth. In cases of extreme tooth discoloration, whitening isn’t always enough and crowns or veneers may be the only choice. But because of the low cost of tooth whitening treatments, it’s usually worth a try.
Teeth whitening methods
Two effective teeth whitening techniques are available today: in-office laser teeth whitening and at-home teeth whitening with custom-fit trays. Both teeth whitening techniques are best performed under your dentist’s supervision to ensure the safest and most dependable results.
-
In-Office Tooth Whitening
methods are performed with bleaching gel and laser light. This is a good method of teeth whitening for sensitive teeth, as the process may be closely monitored by the cosmetic dentist. The teeth are carefully isolated from the lips and gums, and then a bleaching gel is applied to them. A laser is used in conjunction with the gel to accelerate and amplify the tooth whitening process.
-
At-Home Tooth Whitening
are available in a variety of “flavors” for those who are interested in giving whitening a go in the privacy of their home. Your cosmetic dentist can take imprints of your teeth and then make custom-fitted trays for you to take home to complete the tooth whitening process. There are also teeth bleaching kits and other over-the-counter teeth whitening products available to brighten your smile.
Some key benefits of whitening are:
- Corrects brown, yellow, and mottled tooth staining
- Works on people of all ages
- Restores brightness and life to “dull” smiles
Five Reasons Why You May Have a Dry Mouth
Drinking copious amounts of water is good for one’s health.
And, boy howdy, when you’re feeling parched, there’s nothing better than a tall drink of ice-cold water to dampen that dry mouth of yours. But what do you do when you find yourself drinking far more than the recommended amount, and are still feeling as though your mouth is as dry as a desert? There are numerous reasons you could be suffering from dry mouth, ranging from the benign to the serious – let’s take a look at the top five.
Physiologic
Sometimes having a dry mouth is just a normal part of life. Temporary anxiety, open-mouthed breathing, mild dehydration, menopause, pregnancy, and decreases in salivary production due to sleep are all considered physiologic (normal) causes of dry mouth.
Prescription medication
Sixty-three percent of the top 200 most commonly prescribed drugs in the U.S. are known to cause dry mouth. That’s a lot of interference. What’s worse, the higher the number of medications a person takes, the higher the chance of dry mouth. That’s why as we age, we tend to experience more instances of dry mouth. It’s not necessarily age-related, but our consumption of medication may cause this side effect.
Habitual use of alcohol, cigarettes, and/or drugs
Use of any of these products will dry out the oral cavity. No real surprise here.
Chronic Disease
Sjögren’s disease, a chronic autoimmune disease in which white blood cells attack their moisture-producing glands; along with the inflammatory disease, Sarcoidosis; Hepatitis C; and Diabetes, can all cause dry mouth.
Psychogenic or Idiopathic
When symptoms are present without an identifiable cause (idiopathic), or because of psychological causes (psychogenic), they can be difficult to diagnose. If you find yourself with a persistent case of dry mouth that you are unable attribute a cause to, see your doctor for further diagnosis.
Dry mouth can be uncomfortable to live with, and is an indication there is something causing the symptom that requires further examination. As always, with any persistent medical condition it’s important to never rely on self-diagnosis, and to see your doctor for proper evaluation.
Dental Sealants
The deep grooves of teeth present the an ideal environment for bacterial growth
The deep grooves of teeth present the ideal environment for bacterial growth, which can gradually lead to decay. Even if you are vigilant with your dental hygiene habits, bacteria can hide in the recesses where your toothbrush is unable to adequately reach.
Dental sealants have become a popular way of blocking tooth pits and grooves
Dental sealants have become a popular way of blocking tooth pits and grooves to prevent bacterial decay. If you are concerned about the possibility of decay or if you have already developed some small cavities, applying dental sealants may be an ideal solution.
Taking preventative steps now to maintain good dental health
Taking preventative steps now to maintain good dental health can help prevent the need for costly dental treatments and procedures later on.
Sealants are thin liquid coatings that can be applied to the top of a tooth
Sealants are thin liquid coatings that can be applied to the top of a tooth to seal off deep grooved areas. They help to prevent bacteria or other debris from becoming trapped in pitted areas that cannot be easily cleaned.
This type of dental procedure has become increasingly popular
This type of dental procedure has become increasingly popular, and has been shown to be a safe and effective way of stopping tooth decay before it begins.
Children are ideal candidates for sealants
Children are ideal candidates for sealants, because the protective layer can be applied before bacterial decay begins.
Why Doesn't My Insurance Pay for This?
Get Covered A Dental Insurance Glossary
Odds are, you never attended a class called “Dental Insurance 101” during all your schooling
And, whether you’ve been using dental insurance for a while, or are just getting started, there are likely plenty of terms with which you may be unfamiliar.
That’s where we come in!
Below is a list of dental insurance terminology intended to help you best to choose and then use your insurance. This list is by no means comprehensive, but it will certainly get you started with the basics. We hope it helps!
Premium
A premium is the monthly amount you and/or your employer pays the insurance company during your coverage period so that you have insurance coverage.
Employee Contribution (of premium)
The portion of your insurance premium that you, the employee, are responsible for paying in order to obtain coverage.
Benefits
Items and services that your insurance covers.
For example, your insurance likely covers two free exams/cleanings per insurance year, or one every six months.
Benefit Waiting Period
Depending on your insurance, you may have to be enrolled in the same plan for a certain amount of time before it covers a particular service.
For example, a plan may not cover periodontal care until you’ve been enrolled for at least 12 months.
Claim
When you visit your dentist, the office staff will submit a claim to your insurance company. This is a request for insurance to pay for your visit.
Patient portion (of the bill)
After your insurance claim is processed and paid for, there could still be a remaining charge that you have to pay. This will be billed to you directly from the dental office.
Deductible
Some services (like a regular exam/cleaning) may be covered by your insurance, at 100% of their allowable fees. Other services might not be covered until you pay a certain amount per year. This is known as the deductible.
Once your calendar year or insurance year resets, you will begin paying the deductible amount all over again.
Coinsurance
While looking at your plan, if you see “50% coinsurance” next to “Restorations and Sealants,” for example, this means that your insurance will cover 50% of their allowable fee. You would be responsible for paying the difference directly to the dental office.
Copayment/Copay
This is the amount you must pay the dental office during a visit depending on the service(s) you receive.
Depending on your specific insurance plan, you may or may not have a copay.
Annual Maximum
The total amount an insurance company will pay your dental office, on your behalf, during your insurance year. After this amount is paid, you must personally cover any further expenses incurred during the insurance year.
Pre-Treatment Estimate
If you want to see how much a dental procedure or treatment plan will cost you out of pocket, ask your dental office to submit a pre-treatment estimate.
This doesn’t guarantee payment by your insurance company, but it gives you a good idea of what they will cover and what you’ll have to pay.
This list is a good place to start for insurance terminology. Of course, there’s lots more to learn.
For example, what’s the difference between a PPO, HMO, or fee-for-service plan you ask? Click here! Otherwise, we’ve got another great springboard of insurance terms for you here.
When in doubt, call your dental insurance company. They will give you the most accurate and up-to-date information on your specific plan.
You can also call your friendly neighborhood dental office to explain a few things. Don’t be bashful about asking for help! Not many people can say they’re experts in this area!
The One Thing about Flossing Hardly Anyone Does Correctly

Three Steps to a Good Flossing Routine
There are three steps to developing a good flossing routine. Make it easy. Make it fun. And do it correctly. To make it easy, simply leave the floss container on the counter sink for your child to see each time they use the bathroom throughout the day. The constant visual reminder, and keeping the floss at arm’s length will definitely make a difference. Make it fun. Surely, it’s impossible to add any element of “fun” to an oral care routine, right? You’d be surprised – and we’d like to share a method with you that makes flossing fun AND achieves the third step all in one fell swoop. So what is the secret to knocking out two steps in one and doing the one thing with regard to flossing that hardly anyone does correctly? The secret is to …
… curve the floss. Curve the floss?
Employ The Right Method
That’s right, in order for flossing to do its job, you have to guide the floss along the natural curvature of the tooth, downward and below the gum line. Most of us simply slide the floss up and down horizontally between our teeth which completely misses the fundamental objective of flossing. That is, to get plaque below the gum line. Of course, it goes without saying that if most adults don’t floss correctly than our kids aren’t flossing correctly either, so this works for each of us!
Doing so will ward off the plaque that loves to live below the gum line, can’t be reached by a toothbrush, and causes gum disease. Of course, teach your child to always go gentle with the floss, and be sure they’re not forcing it down into the gum line. They shouldn’t ever feel it hit bottom. Instead, it should – and will – “glide” over their teeth. Try it out on your own teeth, and then show your kids how it works. The result will be both that you and your children will spend a lot less time in the hygienist’s chair.
Still worried about how it works? Ask your hygienist to show you and your child the next time you’re each having your teeth flossed in the office, or just pull up a YouTube video on proper flossing … there are bunches of them. And, make it a game! Watch one another floss to see who does it best… give out prizes of your choosing to everyone participating. If you work at finding the best flosser in the family, you’ll find in the end, you all become great flossers! Trust us, you’ll be impressed at just how well this works, and using the technique can actually make flossing fun for everyone in the house!
Are Dental Implants Right for You?
Are Dental Implants Right for You?
Dental implants are part of a long-term replacement solution for missing teeth. They are posts surgically implanted into the jawbone to replace the roots of missing teeth and support dental restorations such as crowns or fixed dentures. You may want to consider dental implants to replace teeth lost due to disease or trauma if:
- You cover your mouth because you are self-conscious about missing teeth
- Your traditional dentures are uncomfortable or slip and shift a lot
- You are unhappy with your partial denture
- You do not want your remaining teeth damaged to anchor a dental bridge
- You have difficulty eating or speaking due to missing teeth
Implants can replace an individual tooth, more than one tooth, or support a full arch of prosthetic teeth resembling dentures but attached permanently to the implants.
Dental implants are made of biocompatible materials that gradually fuse with the surrounding bone. The most common materials are titanium, a lightweight metal used for artificial joint replacements, and zirconia, a durable ceramic used in patients allergic to metal.
Benefits of Dental Implants
Implants are the only permanent, fixed solution for missing teeth. They offer multiple benefits to anyone with missing teeth, including:
- Implants look and feel natural because they fit securely and do not move around in the mouth.
- Unlike dentures and removable bridges, implants do not shift, click, or pinch, preventing embarrassment and pain.
- A single-tooth implant can be placed without damaging adjacent teeth.
- Implants help preserve the jawbone. Without an implant’s stimulation, the jawbone can deteriorate significantly in the first year after tooth loss.
- No dietary restrictions.
- Easy to care for; you brush and floss dental implants like natural teeth.
- Implants do not need to be replaced or repaired. They are the only tooth replacement option that can last a lifetime with proper oral hygiene.
Are You a Candidate for Dental Implants?
If you are in good health and your teeth and gums are healthy, you may be a candidate for dental implants. If you have any cavities or gum disease, such as gingivitis, these must be treated before your dentist can proceed with dental implants.
Some people who are in good health may not have sufficient jawbone mass to support dental implants in the upper or lower jaw. They may be able to get implants, but not until they undergo bone grafting to build up the bony ridge of the jawbone so that it is wide enough and strong enough to support the implants. This may add several months to the dental implant timeline.
Finally, some medical conditions rule out individuals as candidates for implants. Individuals with blood clotting disorders, certain autoimmune diseases, and uncontrolled diabetes are not good candidates because they risk uncontrolled bleeding or implant failure. Heavy smokers also run the risk of implant failure and complications because smoking interferes with the healing process.
Cold Sore Solutions That Actually Work
Cold Sore Solutions That Actually Work
Whether you call them cold sores or fever blisters, if you’re among the more than 40% of Americans who regularly experience this inflammatory viral nuisance, you know they’re anything but a joy to deal with.
Cold Sore Cures
You’ve also probably heard of countless ways to deal with them, from over-the-counter remedies to treatment options that span generations. So, what really works? Well, quite honestly, what “works” when it comes to cold-sores, is management. Specifically, preventing, treating and eliminating the transmission of this most annoying of viruses.
Cold Sore Prevention
The adage “an ounce of prevention is worth a pound of cure,” is certainly true when it comes to cold sores. Knowing what causes them to surface is key. The top two reasons are a weakened immune system, and exposure to rapidly changing weather.
Cold Sore Remedies
To tackle the weather, always keep your preferred brand of lip moisturizer with sunscreen on hand to protect your lips from weather’s effect on your lips. And, to boost your immune system, be sure to get enough sleep and find ways to combat stress in your life.
Also, as with most things in life, what’s good for our waistlines is good for our immune system. Here are some good dietary suggestions for cold sore sufferers:
Dietary Suggestions
Eat Raw, Alkalizing Foods: Fruits and vegetables are super-good for you. Eat as many of them as you enjoy.
Beef-up On Cruciferous Vegetables: Clinical studies are beginning to suggest that veggies like broccoli, cauliflower, cabbage, Brussels sprouts, and kale are of great benefit to cold-sore sufferers.
Avoid Arginine: Cold-sores need the amino acid arginine to grow, so if you can limit the excess intake of this amino acid, you may be able to keep frequent outbreaks at bay. Nuts, chocolate, oats, and some protein shakes are high in arginine and can be major cold-sore triggers.
Cold Sore Treatment and Remedies
Preventing a cold sore from appearing is indeed your best medicine, and if you pay attention to what your body tells you, it is possible to dramatically reduce outbreaks. When a cold-sore does gift you with its presence, though, here are a few things you can do to minimize its pain, size and duration.
Cold-Sore Management
Ice It! At the first sign of tingling, get thee to an ice cube, wrap it in a paper-towel, and place it on your lip where you feel the cold-sore coming on. Often two back-to-back applications of an ice cube until it melts can dramatically reduce the pain and swelling that accompanies the sore.
Slather It? Not Now, But Later. Cold sores love warm, moist environments, and this is precisely the environment you present to a cold-sore when you slather it in cream for days on end. You’re best to let it dry out to the point where it is no longer painful, and then begin applying cream or lip balm to minimize splitting. As the cold sore resolves itself, keep your lips moist to prevent bleeding, which also aids in the healing at this stage.
Eliminate Transmission of Cold Sores: Avoid sharing food, utensils, towels, toothbrushes, or any other item that come in contact with your mouth. Also, be sure to avoid touching the cold sore and then later touching your eyes or genital area. In fact, your best course of action is to avoid touching your mouth at all during an outbreak, and not again until after the scab has dropped off completely, and healed over. This can take some weeks, as you know.
Kissing, and other aspects of intimacy that involve your mouth should be avoided entirely. Wash your hands often – this cannot be stressed enough to avoid spreading the virus. Having a cold sore is not the end of the world. Nine out of ten of all people get at least one cold sore in their life, so there is no need to hide or be embarrassed. Understand your triggers, find a solution that works, don’t spread the virus, and stay healthy!
Stressed Out about a Gummy Smile Did You Know it Can Be Corrected

The amount of gum tissue we possess, just like how much hair we have on our heads, is merely a matter of personal anatomy – some of us just have more of it than others. If you are unhappy with your smile though, and consider yourself to have “too much” gum tissue, there are a few ways to relieve you of a gummy smile. Let’s take a look at the three most common options:
Gingivectomy (Gum Lift, Gum Contouring)
The most common and speediest solution for revitalizing a gummy smile is a gingivectomy. A gingivectomy is the medical term for the surgical removal of gum tissue from the crown of the tooth. It can be done with a scalpel, an electrosurgery unit, lasers or diamond dental burs. There’s some art to this procedure, since your dentist effectively “carves” away the excessive tissue, reshaping the landscape of your smile so it conforms to your desired result. The procedure is done under local anesthetic and takes only a few minutes to an hour to complete depending on the number of teeth to be done.
Lip Repositioning
This one might sound a bit scary, but other than post surgical swelling and some initial tightness, it can be a good solution if your gumminess comes from how high your lip raises when smiling, instead of excessive gingiva.
In this procedure, a small horizontal section of tissue inside your upper lip is removed, then stitched back together in what is effectively a “lower” position. If you can imagine having a cut in your skin where some of the skin tissue in the middle of the cut is lost, and the remaining “ends” of the skin are stitched back together, that is essentially what happens in a lip positioning. Your lip isn’t actually lowered, it’s just that some of the movement of your top lip is restricted so it doesn’t raise too high and show too much gum. Surgery only lasts about 45 minutes, and the results are immediate.
Crown Lengthening
With the word “lengthening” in the name of this procedure, you may think it requires some sort of painful stretching of the tooth’s crown to make it longer. Thankfully, that’s not what happens. Instead, in this surgery a dentist would make an incision in the gum tissue, creating a “flap” that can be folded downward, exposing the bone that encases your teeth. A portion of that bone would then be shaved down few millimeters and the gum flap sutured back into place. At this point, however, because the bone height is lower than it was previously, the gum tissue would rest at a lower height, leaving more of the crown visible when smiling. This would make it appear as though the crown were “longer” and thus the name – “crown lengthening” is given to this procedure. While crown lengthening is a means to correct a gummy smile, many dentists recommend orthodontic treatment, instead (which, over time actually does pull the crown down a few millimeters), because it doesn’t require surgery, or the permanent removal of bone tissue.
Modern dental surgery can really do wonders for our smiles in a multitude of ways. If you’re concerned about how much gum you are flashing each time you smile, or have stopped smiling all together, have a chat with your dentist. You might be surprised at just how quickly we can get you back to smiling widely again!